Prostate Health, Testosterone And TRT – The Complete Guide
Last Updated On April 22, 2025
Contents
- Introduction
- 1. The Basics: How Testosterone And The Prostate Are Connected
- 2. PSA Levels, Prostate Cancer, And Testosterone
- 3. Enlarged Prostate (BPH), Urinary Symptoms, And TRT
- 4. Lifestyle, Diet, And Supplements For Prostate Health
- 5. Prostate Health Monitoring And Preventative Care
- 6. Medical Treatments And Prostate Health
- 7. Misconceptions And Myths About Prostate Health
- Final Thoughts
Introduction
Prostate health is one of the most commonly discussed concerns for men on testosterone replacement therapy (TRT). Many TRT users worry about whether testosterone affects the prostate, increases PSA levels, worsens urinary symptoms, or raises the risk of prostate cancer. These concerns are often fueled by outdated medical beliefs, conflicting research, and well-intentioned but misinformed advice from doctors.
For decades, the medical community widely believed that testosterone fueled prostate cancer. This idea was based on the assumption that since androgen deprivation therapy (reducing testosterone to castrate levels) was used as a treatment for advanced prostate cancer, testosterone itself must be a risk factor. However, modern research, led by experts in the field, has repeatedly challenged this belief. Yet, despite strong scientific evidence, the fear surrounding TRT and prostate health remains.
Prostate Health On TRT: Essentials Summary
- Does TRT cause prostate cancer? No, studies show no direct link between TRT and prostate cancer risk.
- Can TRT raise PSA levels? Yes, but often within a normal range. A rapid or extreme rise should be evaluated.
- Does TRT make BPH worse? It depends. Some men see minor prostate growth, but others report better urinary function.
- Should you block DHT with finasteride? This is debated. Blocking DHT may reduce prostate size but can come with side effects.
1. The Basics: How Testosterone And The Prostate Are Connected
What Is The Prostate, And Why Is It Important?
The prostate is a small, walnut-shaped gland located just below the bladder. It surrounds the urethra and plays a key role in male reproductive function by producing prostate fluid, a component of semen that helps sperm survive and function properly.
Beyond reproduction, the prostate also affects urinary function. Because the urethra passes through it, changes in prostate size or inflammation can lead to urinary symptoms such as frequent urination, weak flow, or difficulty emptying the bladder.
Many men begin experiencing prostate-related issues as they age, with conditions such as benign prostatic hyperplasia (BPH) and prostatitis becoming more common. However, prostate cancer is often the biggest concern, especially for men on TRT who have heard that testosterone might contribute to its development.
How Testosterone Affects The Prostate: Separating Fact From Fiction
One of the most persistent beliefs in medicine is that testosterone fuels prostate cancer. This idea has been around for decades, but modern research has shown that it is not supported by scientific evidence.
The fear comes from the fact that doctors treat advanced prostate cancer by suppressing testosterone levels to near-zero (androgen deprivation therapy). The assumption was that if lowering testosterone slows cancer, then raising testosterone must accelerate it. However, research from leading experts has shown that this is an oversimplification of prostate cancer biology.
- Prostate cells require some testosterone to function, but beyond a certain threshold, additional testosterone does not stimulate more growth.
- The “saturation model,” developed by Dr. Abraham Morgentaler and others, explains why once testosterone levels reach normal physiological ranges, increasing them further has little to no effect on prostate cancer growth.
- Men with low testosterone are not protected from prostate cancer. In fact, some research suggests that men with lower testosterone levels may have more aggressive prostate cancer.
Does TRT Cause Prostate Cancer? Debunking The Myth

The belief that TRT increases the risk of prostate cancer is based on outdated ideas that have been widely challenged by modern research. No well-conducted study has shown that TRT increases the risk of developing prostate cancer.
- A 2016 study in the New England Journal of Medicine found no link between TRT and increased prostate cancer risk.
- A 2017 meta-analysis of multiple studies confirmed that men on TRT did not have a higher incidence of prostate cancer than men not using testosterone.
- Data from long-term observational studies show that TRT does not accelerate prostate cancer growth in men who already have it.
Despite this, many doctors continue to cite old research as a reason to avoid TRT in men concerned about prostate health. The difference between mainstream medical advice and expert perspectives on this topic will be explored in greater depth later in this guide.
The Morgentaler Saturation Model – Why TRT Does Not Fuel Prostate Cancer

Dr. Abraham Morgentaler, a urologist and leading researcher in the field of testosterone and prostate health, developed the Saturation Model to explain why TRT does not increase the risk of prostate cancer.
The Saturation Model states that prostate tissue only requires a small amount of testosterone to function properly. Once that baseline amount is met, increasing testosterone further does not stimulate additional prostate growth.
- Think of it like watering a plant: A small amount of water helps the plant grow, but flooding it with excess water won’t make it grow any faster.
- This explains why TRT does not “fuel” prostate cancer, as once the prostate has enough testosterone, adding more has little effect.
This theory has been supported by multiple studies that have examined men on TRT and found no increased risk of prostate cancer progression or incidence.
DHT, Estrogen, And Prostate Health – What’s The Real Culprit?
While testosterone often takes the blame for prostate-related issues, other hormones like dihydrotestosterone (DHT) and estrogen have been investigated for their potential roles in prostate enlargement and inflammation.
DHT is a potent androgen derived from testosterone through the action of the enzyme 5-alpha reductase. It is necessary for normal prostate function and development, and its involvement in benign prostatic hyperplasia (BPH) has been widely studied. However, not all research supports the idea that DHT is the primary driver of prostate growth, and in some cases, suppressing DHT does not lead to significant symptom improvement.
Estrogen has been discussed as a potential factor in prostate inflammation, but the scientific evidence remains inconclusive. Some researchers have suggested that estrogen metabolites, rather than total estrogen levels, may play a role in prostate inflammation. However, this hypothesis is largely based on animal studies and has not been definitively proven in human trials.
Some TRT users have reported worsened prostate symptoms when estradiol levels are elevated, but others have not observed any negative effects. The variation in individual responses suggests that other factors, such as metabolic health, chronic inflammation, and overall hormone balance, may play a greater role than estrogen alone in prostate health.
Given the lack of strong clinical evidence, estrogen’s role in prostate inflammation remains speculative. At this time, the focus should remain on well-documented factors such as PSA trends, prostate volume changes, and symptom progression rather than theoretical concerns about estrogen dominance.

Hormone Balance Beyond Testosterone: What Really Affects Prostate Health?
Testosterone plays a role in prostate health, but other hormones—DHT, estrogen, SHBG, cortisol, and insulin—also have a major impact. Understanding how these interact is key to optimizing prostate function and preventing issues like BPH and prostate cancer.
Key Hormones That Influence Prostate Health
- Dihydrotestosterone (DHT)
- Often blamed for BPH, but moderate DHT levels are necessary for prostate function.
- Excessive DHT may worsen BPH symptoms, but completely blocking it (via finasteride or dutasteride) can cause hormonal imbalances and sexual dysfunction.
- Estrogen (E2 & Estrone)
- High estrogen is linked to increased BPH risk and prostate inflammation.
- Men with metabolic syndrome often have higher estrogen due to excess body fat.
- Balancing estrogen with testosterone is critical—too much suppression can cause issues, but letting it rise unchecked can exacerbate prostate growth.
- Sex Hormone Binding Globulin (SHBG)
- SHBG binds to testosterone and DHT, controlling their availability.
- High SHBG means less free testosterone, which can contribute to low libido, poor prostate function, and metabolic dysfunction.
- Low SHBG is linked to insulin resistance, which can negatively affect prostate health.
- Cortisol & Stress Response
- Chronic stress raises cortisol levels, which can increase systemic inflammation and worsen prostate conditions.
- High cortisol suppresses testosterone, potentially leading to weaker immune function and increased oxidative stress.
- Insulin & Prostate Growth
- High insulin and insulin-like growth factor 1 (IGF-1) promote prostate enlargement.
- Diabetics and men with metabolic syndrome have higher rates of BPH and aggressive prostate cancer.
- Reducing sugar and processed carbs helps regulate insulin levels and may reduce prostate enlargement risk.
The Importance of Balancing These Hormones
- Testosterone alone isn’t the issue—prostate health depends on the balance of DHT, estrogen, SHBG, cortisol, and insulin.
- Men with metabolic dysfunction and high estrogen levels are at greater risk for prostate problems.
- TRT can help restore balance, but monitoring estrogen, SHBG, and insulin resistance is essential.
Does High Testosterone Or DHT Cause An Enlarged Prostate?
BPH is a common condition in older men, and since it involves prostate growth, testosterone and DHT have often been assumed to play a role. However, studies show that the relationship is not straightforward. BPH can occur in men with both high and low testosterone levels, suggesting that testosterone alone is not the driving factor.
Some experts argue that testosterone does not cause BPH but rather that declining testosterone and an imbalance between androgens and estrogens contribute to prostate enlargement. This is why some men on TRT actually experience improved urinary symptoms rather than worsening ones.
DHT is sometimes blamed for prostate growth, but blocking it through medications like finasteride or dutasteride does not necessarily improve symptoms in all cases. Many men who suppress DHT experience sexual dysfunction and mood disturbances without significant benefits to urinary health. Thus, whether high DHT is a direct cause of BPH remains an open debate.
Mainstream Medical Advice vs. Expert Perspective: Does TRT Impact The Prostate?
For years, mainstream medical guidance has cautioned against TRT for men with prostate concerns due to fears of prostate cancer or worsening BPH. Many doctors still hesitate to prescribe TRT to men with elevated PSA levels or a history of prostate disease.
However, experts in the field of hormone optimization argue that this perspective is outdated. Newer research indicates that TRT does not increase the risk of prostate cancer and may even be beneficial for prostate health. Some key points of difference between mainstream and expert perspectives include:
- Mainstream View: TRT increases PSA and prostate size, leading to a higher risk of prostate issues.
- Expert View: PSA increases on TRT are typically mild and not indicative of cancer. Prostate size may increase slightly, but this does not always correlate with worsening urinary symptoms.
- Mainstream View: Lowering testosterone is necessary to reduce prostate cancer risk.
- Expert View: Low testosterone may contribute to more aggressive prostate cancer. Restoring testosterone to normal levels is beneficial for overall health.
Understanding PSA Levels On TRT: When To Be Concerned
PSA (prostate-specific antigen) is a protein produced by the prostate and used as a marker for prostate health. PSA levels can rise due to a variety of factors, including prostate cancer, BPH, prostatitis, and even recent sexual activity or exercise.
For men on TRT, PSA levels may increase slightly when starting therapy. However, a mild increase does not necessarily indicate cancer. Significant spikes (greater than 1.4 ng/mL per year) warrant further investigation. Many doctors overreact to PSA fluctuations, sometimes taking men off TRT unnecessarily.
A better approach is to monitor PSA trends over time rather than react to single measurements. A prostate MRI or free PSA ratio test can provide a clearer picture before jumping to conclusions.
Can TRT Cause Prostate Enlargement (BPH)?
TRT does not inherently cause prostate enlargement, but it may increase prostate volume slightly in some men. However, this does not always lead to worsening urinary symptoms. Some men on TRT even report improved urinary function, possibly due to the strengthening of bladder and pelvic muscles.
Men with pre-existing BPH should monitor symptoms closely while on TRT. If urinary symptoms worsen, adjusting TRT dosage or managing estrogen levels may help. While some discussions suggest that estrogen may play a role in prostate inflammation and growth, there is no strong clinical evidence confirming this as a primary factor.

Can Testosterone Improve Prostate Function In Some Men?
Emerging research suggests that TRT may actually support prostate health in certain cases. Some studies indicate that men with low testosterone are more likely to experience severe urinary symptoms and that restoring testosterone to optimal levels can improve bladder control and prostate function.
Additionally, men with low testosterone have been found to have a higher likelihood of developing more aggressive prostate cancer. This challenges the traditional belief that testosterone is inherently harmful to the prostate.
TRT, Finasteride, And Prostate Health – Should You Block DHT?

Finasteride and dutasteride are 5-alpha reductase inhibitors that block the conversion of testosterone into DHT. They are commonly used to treat BPH and male pattern baldness. However, blocking DHT comes with potential downsides, particularly for men on TRT.
Some concerns with finasteride include:
- Sexual dysfunction: Many men report reduced libido and erectile difficulties.
- Mood and cognitive issues: Some users experience brain fog, anxiety, or depression.
- Post-Finasteride Syndrome (PFS): A subset of men experience long-term side effects even after stopping the drug.
- Lowered PSA readings: Finasteride artificially reduces PSA levels, which can mask early signs of prostate cancer.
Some experts believe that blocking DHT is unnecessary for many men on TRT and may reduce the benefits of testosterone therapy. They argue that balancing estrogen and addressing inflammation may be more effective for prostate health than suppressing DHT.
Key Takeaways
- Testosterone is not the primary cause of prostate cancer or BPH. Modern research challenges old assumptions linking testosterone to prostate disease.
- DHT and estrogen may play a more significant role in prostate health. While DHT has been associated with prostate growth, estrogen imbalance could be a bigger factor in inflammation and enlargement.
- PSA increases on TRT are not always concerning. Small fluctuations are normal, but rapid rises should be monitored with additional testing.
- Blocking DHT with finasteride is controversial. While it can shrink the prostate, it may come with unwanted side effects and is not necessary for all men.
2. PSA Levels, Prostate Cancer, And Testosterone

Understanding PSA Levels – Why PSA Testing Has Been A Public Health Disaster
Prostate-specific antigen (PSA) testing has been a cornerstone of prostate cancer screening for decades. However, mounting evidence has shown that widespread PSA screening has led to a public health crisis of overdiagnosis and overtreatment. Originally developed to monitor prostate cancer progression, PSA testing was never intended as a first-line diagnostic tool for detecting cancer. The medical community’s reliance on PSA testing has caused millions of men to undergo unnecessary biopsies, treatments, and even surgeries—many of which resulted in lasting complications.
PSA levels can rise due to various non-cancerous factors, including benign prostatic hyperplasia (BPH), prostatitis, infections, sexual activity, and even recent exercise. Despite this, many doctors still interpret elevated PSA levels as an indicator of prostate cancer, leading to a cascade of interventions that may not be necessary.
PSA Interpretation & Bloodwork: What Your Numbers Really Mean
Most men are told that a high PSA (Prostate-Specific Antigen) means possible prostate cancer, but PSA alone is an unreliable diagnostic tool. To interpret PSA properly, doctors should analyze multiple PSA-related factors rather than relying on a single number.
Key PSA Metrics That Matter
- Total PSA – The overall amount of PSA in the blood. A “normal” PSA is often considered under 4.0 ng/mL, but this varies by age and individual risk factors.
- PSA Velocity – The rate at which PSA rises over time. A rapid increase (>0.75 ng/mL per year) is more concerning than a single elevated reading.
- PSA Density (PSAD) – PSA levels divided by prostate volume (measured via ultrasound or MRI). A PSAD above 0.15 ng/mL/cm³ may indicate higher risk.
- Free-to-Total PSA Ratio – The percentage of PSA that is “free” (not bound to proteins). A higher free PSA (>25%) is reassuring, while lower free PSA (<10%) suggests a higher cancer risk.
- Age-Specific PSA Ranges – PSA naturally increases with age. Instead of a fixed 4.0 ng/mL threshold, a PSA of 2.5 ng/mL at 40 may be concerning, while 5.0 ng/mL at 70 may be normal.
- Inflammation & PSA Spikes – PSA levels fluctuate due to:
- Recent ejaculation (can temporarily raise PSA for 24-48 hours)
- Biking or prolonged sitting (pressure on the prostate)
- Infections or prostatitis (temporary PSA elevations)
- BPH (Benign Prostatic Hyperplasia) (can elevate PSA without cancer)
When Should You Worry About PSA?
- A single elevated PSA reading isn’t enough – always check PSA trends over time.
- A consistently rising PSA (>0.75 ng/mL per year) should prompt further evaluation.
- Low free PSA (<10%) + high PSA density (>0.15 ng/mL/cm³) suggests higher risk.
- A sudden PSA spike without other symptoms might be caused by prostatitis, irritation, or BPH rather than cancer.
Why PSA Alone Is A Flawed Diagnostic Tool
- Many men with “high PSA” (above 4.0 ng/mL) don’t have cancer.
- Many men with low PSA still develop prostate cancer.
- Instead of panicking over a single PSA number, look at the complete picture: PSA trends, free-to-total PSA ratio, prostate size, and additional imaging tests like multiparametric MRI.
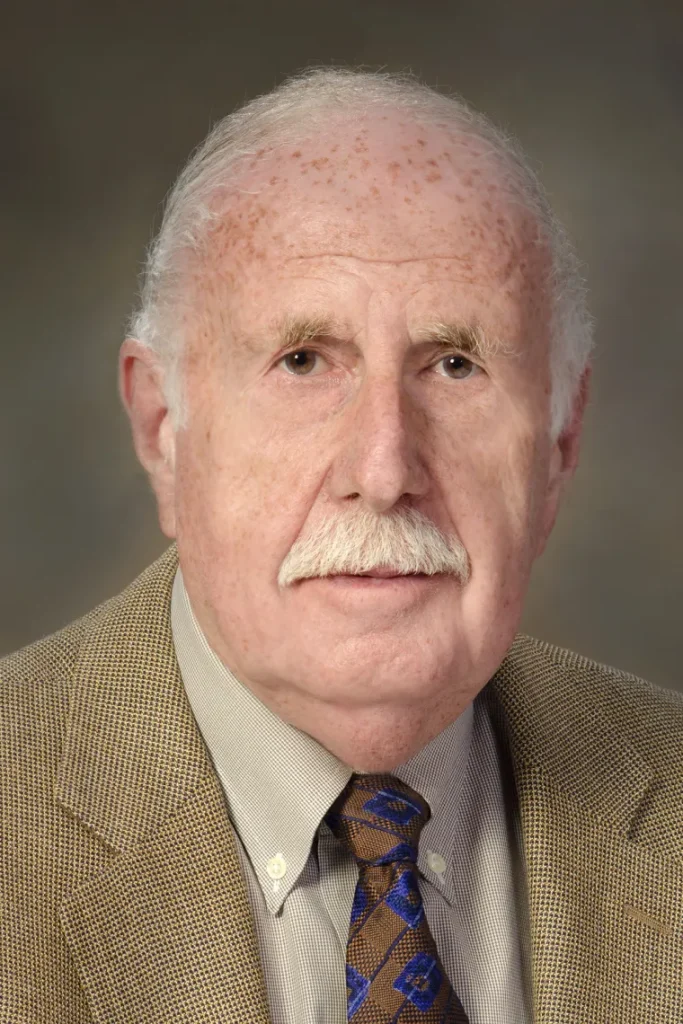
The PSA Test Was Never Meant For Cancer Screening – What Experts Say
Dr. Richard Ablin, the scientist who discovered PSA, has been vocal about the misuse of PSA testing. In his book The Great Prostate Hoax, he explains how the test was hijacked by the medical industry and turned into a billion-dollar business despite its lack of reliability as a standalone diagnostic tool. According to Ablin and other leading experts, PSA testing should be reserved for monitoring already-diagnosed prostate cancer rather than as a universal screening method.
The U.S. Preventive Services Task Force (USPSTF) downgraded PSA screening recommendations after studies showed that widespread testing led to minimal reductions in prostate cancer mortality while significantly increasing rates of overdiagnosis and overtreatment. Many men who underwent prostate cancer treatment based on PSA results later suffered from erectile dysfunction, urinary incontinence, and other complications—despite having slow-growing cancers that may never have caused harm.
Why PSA Alone Is Not A Reliable Cancer Test
One of the biggest flaws of PSA screening is that it cannot distinguish between aggressive prostate cancer and slow-growing, indolent tumors that pose little threat. Many older men develop prostate cancer at some point in their lives, but the vast majority will never experience symptoms or require treatment. PSA testing often identifies these low-risk cases, leading to unnecessary anxiety and invasive procedures.
False positives are another major issue. Elevated PSA levels frequently trigger unnecessary biopsies, which carry risks of infection, bleeding, and complications. Meanwhile, some aggressive cancers do not produce significant PSA elevations, leading to false negatives that provide false reassurance. These limitations make PSA testing an unreliable tool when used in isolation.
Can PSA Levels Increase On TRT Without Indicating Cancer?
Testosterone replacement therapy (TRT) has been falsely blamed for increasing PSA levels and fueling prostate cancer. However, research shows that while TRT can cause slight PSA elevations in some men, these increases are typically minor and do not indicate cancer.
Dr. Abraham Morgentaler’s research found that PSA levels in men on TRT tend to stabilize after an initial increase, and long-term TRT does not raise the risk of prostate cancer. Additionally, studies have shown that PSA levels in hypogonadal men often normalize once testosterone levels are restored, suggesting that low testosterone may actually contribute to prostate dysfunction.
How To Monitor PSA While On TRT Without Overreacting
Men on TRT should monitor their PSA levels, but it is critical to interpret results in context. Here are key factors to consider:
- Baseline PSA Before Starting TRT: Having a pre-TRT PSA level provides a reference point for future comparisons.
- Rate Of PSA Change Over Time: A gradual increase may be benign, while a rapid or significant rise warrants further evaluation.
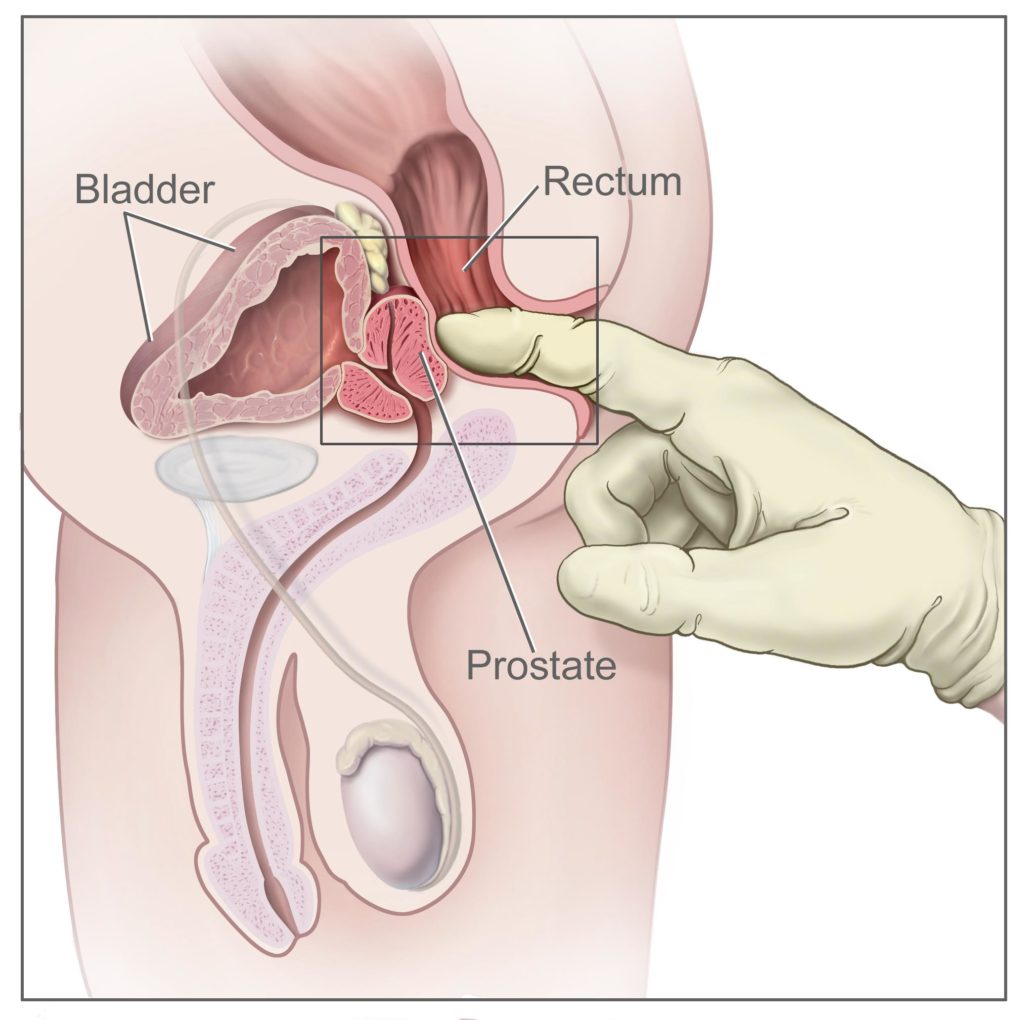
- Symptoms And Additional Testing: PSA levels should not be the sole factor in deciding further testing—DRE (digital rectal exam), MRI, and other assessments should be considered.
- Inflammation And Transient PSA Spikes: Infections, prostatitis, and even recent ejaculation can temporarily raise PSA levels. Retesting after a few weeks can confirm if an increase was transient.
Prostate Cancer And PSA Testing – How It Led To Overdiagnosis And Overtreatment

The aggressive push for PSA screening in the 1990s resulted in a surge of prostate cancer diagnoses. Many of these cases were clinically insignificant, yet men were subjected to biopsies, radiation, and radical prostatectomies. The side effects of overtreatment—impotence, incontinence, and reduced quality of life—far outweighed any potential benefits for those with slow-growing tumors.
Recent research supports a more conservative approach, emphasizing active surveillance rather than immediate intervention for low-risk prostate cancers. This shift aligns with expert perspectives that advocate for a nuanced, individualized approach to prostate health monitoring rather than indiscriminate PSA screening.
Mainstream vs. Expert Perspectives: Is PSA Screening Necessary For All Men?

Mainstream medical guidelines often promote routine PSA screening for men over 50, but many experts challenge this blanket recommendation.
- Mainstream View: PSA screening can help catch cancer early, potentially reducing mortality.
- Expert Perspective: The harms of overdiagnosis and overtreatment often outweigh the benefits, and PSA testing should be used selectively based on risk factors and individual health status.
Organizations like the USPSTF now advise against routine PSA screening for all men and instead recommend shared decision-making between patients and doctors. High-risk individuals, such as those with a family history of aggressive prostate cancer, may still benefit from screening—but it should be done with full awareness of its limitations.
Case Study: Men On TRT Who Developed Prostate Cancer – What Happened Next?
Several case studies have examined men on TRT who were later diagnosed with prostate cancer. In many instances, these men safely resumed TRT after treatment without adverse effects.
Dr. Morgentaler’s research highlights that TRT does not appear to fuel prostate cancer growth once treatment is completed, challenging the outdated belief that testosterone is a primary driver of prostate cancer. In fact, some men experience improved quality of life by restoring testosterone levels post-treatment under medical supervision.
Key Takeaways
- PSA testing was never designed to be a first-line screening tool for prostate cancer, and its widespread use has led to overdiagnosis and overtreatment.
- Many factors besides cancer can cause PSA levels to rise, including BPH, prostatitis, infections, and even sexual activity.
- TRT can cause minor PSA elevations, but these are usually not indicative of cancer and tend to stabilize over time.
- Monitoring PSA while on TRT requires context—baseline values, trends over time, and additional diagnostic tools should all be considered before making any conclusions.
- The mainstream medical approach to PSA screening has shifted toward more selective use, with experts advocating for risk-based screening rather than routine testing for all men.
- Many men who develop prostate cancer while on TRT have resumed therapy safely after treatment, challenging the outdated belief that testosterone fuels cancer growth.
Conclusion
PSA testing remains a controversial tool in prostate health management. While it can be useful in specific situations, its widespread use for routine screening has led to overdiagnosis and unnecessary treatments that have harmed countless men. For those on TRT, monitoring PSA levels should be done carefully and in context, with an understanding that minor fluctuations do not necessarily indicate cancer.
The key takeaway: PSA testing should not be feared, but it should also not be blindly trusted. A more nuanced approach—considering symptoms, risk factors, and additional diagnostic tools—is essential for making informed decisions about prostate health on TRT.
3. Enlarged Prostate (BPH), Urinary Symptoms, And TRT

Symptoms Of An Enlarged Prostate (BPH) And How It Affects Men On TRT
Benign prostatic hyperplasia (BPH) is a common condition in aging men, characterized by the gradual enlargement of the prostate gland. This can lead to urinary symptoms that affect daily life, including:
- Frequent urination, especially at night (nocturia)
- Weak urine stream or difficulty starting urination
- Urgency and inability to hold urine
- Incomplete bladder emptying
- Increased risk of urinary tract infections (UTIs)
For men on TRT, concerns often arise about whether testosterone can exacerbate BPH symptoms. Understanding the relationship between TRT and prostate size is crucial for managing urinary health.
Does TRT Make BPH Worse?

One of the most debated topics in men’s health is whether TRT contributes to prostate enlargement. Historically, doctors feared that increasing testosterone levels could accelerate prostate growth, but modern research provides a more nuanced perspective:
- TRT may cause a slight increase in prostate volume, but this does not necessarily lead to worsening urinary symptoms.
- Some men experience improvement in urinary function on TRT, likely due to testosterone’s role in maintaining muscle tone in the bladder and pelvic floor.
- Studies show that TRT does not significantly increase BPH symptoms when properly monitored.
Ultimately, the impact of TRT on BPH varies from person to person, and careful symptom tracking is necessary.
BPH And DHT – Is DHT Really The Problem?
Dihydrotestosterone (DHT), a potent androgen derived from testosterone, has long been associated with prostate growth. Medications like finasteride and dutasteride work by inhibiting DHT production to shrink the prostate. However, the relationship between DHT and BPH is more complex than it seems:
- DHT is necessary for normal prostate function, but excessive levels might contribute to enlargement.
- Blocking DHT does not always relieve BPH symptoms and can lead to sexual dysfunction and mood issues.
- Some experts argue that inflammation and metabolic factors play a bigger role in BPH than DHT alone.
Can TRT Worsen Urinary Symptoms?

While some men on TRT report mild increases in urinary frequency, others experience no changes or even improvement. Several factors influence this outcome:
- Baseline Prostate Health – If a man already has moderate to severe BPH, any increase in prostate size could worsen symptoms.
- Hormonal Balance – Imbalances between testosterone, DHT, and estrogen may contribute to prostate inflammation and urinary discomfort.
- Overall Metabolic Health – Obesity, insulin resistance, and chronic inflammation may be bigger contributors to worsening urinary symptoms than TRT.
TRT & Lower Urinary Tract Symptoms (LUTS): Does It Help or Hurt?
Lower urinary tract symptoms (LUTS)—which include frequent urination, urgency, weak stream, and nocturia—are often associated with BPH. Some doctors wrongly assume TRT makes these symptoms worse, but the relationship is more complex.
How TRT Affects Urinary Symptoms
- Testosterone May Improve Bladder Function
- Some men experience better urinary flow and bladder control on TRT, possibly due to testosterone’s role in muscle tone and nerve function.
- Estrogen & DHT Play a Bigger Role
- LUTS is often driven by high estrogen or DHT imbalances, not testosterone itself.
- Men on TRT who convert too much T to E2 may experience worsened LUTS if estrogen remains unchecked.
- TRT Can Reduce Inflammation
- Low testosterone is linked to higher inflammation, which may worsen bladder irritation and prostate swelling.
Bottom Line:
- TRT does not inherently worsen LUTS, and in some cases, it improves symptoms.
- If LUTS worsens on TRT, check estrogen and DHT levels first.
Prostate Size And Aging – Why Every Man’s Prostate Grows Over Time
As men age, the prostate naturally enlarges due to hormonal changes. This is a normal part of aging, but factors such as genetics, diet, and overall health influence the rate of enlargement. While many men develop BPH, only some experience significant symptoms requiring treatment.
Does Estrogen Contribute To BPH And Prostate Inflammation?
Estrogen is often overlooked in discussions about prostate health. While traditionally considered a female hormone, men produce and require estrogen for various physiological functions. However, estrogen alone is not the primary driver of BPH or prostate inflammation. Instead, its effects depend on overall hormonal balance and systemic inflammation.
- Excess estrogen, when out of proportion with testosterone, may contribute to prostate inflammation in some men.
- Inflammation and metabolic dysfunction appear to be stronger contributors to BPH than estrogen alone.
- Managing estrogen levels within a balanced range, rather than excessively lowering it, is key for optimal prostate health.
Prostatitis: A Hidden Cause of Prostate Pain & Urinary Symptoms

Many men assume that frequent urination and discomfort are due to BPH, but in some cases, the real cause is prostatitis—inflammation of the prostate.
Types of Prostatitis
- Acute Bacterial Prostatitis – A sudden bacterial infection causing fever, pain, and urinary retention. Requires immediate antibiotics.
- Chronic Bacterial Prostatitis – Long-term, low-grade infection leading to recurrent urinary symptoms.
- Chronic Pelvic Pain Syndrome (CPPS) – The most common form, often linked to stress, muscle tension, and inflammation rather than infection.
Symptoms of Prostatitis
- Pain in the perineum, lower back, or testicles
- Burning or discomfort when urinating
- Frequent urination, urgency, or incomplete emptying
Natural & Medical Treatments
- Anti-inflammatory diet, stress management, and pelvic floor therapy help non-bacterial cases.
- Antibiotics only work for bacterial prostatitis—many cases are not bacterial and should not be overtreated with antibiotics.
Do 5-Alpha Reductase Inhibitors (Finasteride/Dutasteride) Shrink The Prostate?
5-alpha reductase inhibitors (5-ARIs) like finasteride and dutasteride work by blocking the conversion of testosterone to DHT, leading to prostate shrinkage over time. However, these medications have potential downsides:
- Reduced libido and erectile dysfunction
- Mood and cognitive side effects
- Lowered PSA readings, which can mask early signs of prostate cancer
For men on TRT, blocking DHT may diminish some of the benefits of testosterone therapy. The decision to use 5-ARIs should be weighed carefully against potential risks.
Why Prostate Issues Can Lead to Bladder & Kidney Problems
An enlarged prostate (BPH) or chronic inflammation doesn’t just affect urination—it can impact the bladder and kidneys if left untreated.
How BPH & Prostatitis Affect Bladder & Kidney Function
- Urinary Retention Can Lead to Bladder Damage
- If the prostate blocks urine flow, the bladder has to work harder, leading to muscle thickening and loss of function over time.
- Chronic Urine Backflow Can Damage the Kidneys
- Severe BPH or untreated urinary retention can cause urine to back up into the kidneys, potentially leading to hydronephrosis (swelling of the kidneys) or kidney failure.
- Bladder Overactivity from Chronic Inflammation
- Prostatitis and chronic irritation can make the bladder overactive, leading to frequent urination, urgency, and incomplete emptying.
Prevention & Management
- Address BPH early to prevent long-term bladder dysfunction.
- Ensure complete bladder emptying—intermittent self-catheterization may be necessary for severe cases.
- Check kidney function (creatinine, eGFR) if BPH is severe.
How To Reduce Nocturia (Frequent Nighttime Urination) On TRT

Nocturia, or frequent nighttime urination, can significantly disrupt sleep. Several strategies may help reduce this symptom for men on TRT:
- Adjusting fluid intake in the evening
- Maintaining balanced hormone levels, including testosterone and estrogen
- Managing metabolic health through diet and exercise
- Using alpha-blockers or herbal supplements like saw palmetto if necessary
Pelvic Floor Therapy: An Overlooked Solution for Urinary Symptoms

Many men assume BPH or prostate enlargement is the cause of their urinary issues, but in some cases, pelvic floor dysfunction is the real problem.
How Weak or Overactive Pelvic Muscles Affect Urination
- Tight pelvic floor muscles can mimic BPH symptoms, making urination difficult.
- Weak pelvic floor muscles lead to poor bladder control and post-void dribbling.
- Chronic stress & tension cause pelvic floor dysfunction, often mistaken for prostatitis or BPH.
Pelvic Floor Exercises for Prostate & Urinary Health
- Kegel Exercises – Strengthens the pelvic muscles to improve bladder control.
- Stretching & Deep Breathing – Helps relax tight pelvic muscles.
- Physical Therapy – A trained pelvic floor therapist can diagnose and treat dysfunction.
When to Consider Pelvic Floor Therapy
- If urinary symptoms persist despite normal prostate size and function.
- If you have pelvic pain, tightness, or discomfort that worsens with stress.
- If traditional BPH treatments aren’t working.
Does Cycling Or Sitting Too Much Increase PSA?

Prolonged pressure on the prostate, such as from long periods of cycling or sitting, may cause temporary PSA elevations and mild discomfort. However, these effects are usually transient and do not indicate serious prostate problems.
Key Takeaways
- BPH is common in aging men, but TRT does not necessarily worsen symptoms.
- DHT is often blamed for BPH, but its role is complex, and blocking it is not always beneficial.
- Elevated estrogen levels alone are not a primary cause of BPH, but an imbalance between testosterone and estrogen may contribute to inflammation in some men.
- Men with pre-existing urinary symptoms should monitor changes closely while on TRT.
- 5-ARIs like finasteride can shrink the prostate but come with side effects.
- Lifestyle adjustments can help reduce urinary symptoms, especially nocturia.
Conclusion
BPH and urinary symptoms are concerns for many men, but the relationship between TRT and prostate health is not as straightforward as once believed. While TRT may cause mild prostate enlargement, it does not inherently worsen urinary symptoms in all men. Managing hormone balance, metabolic health, and lifestyle factors can go a long way in maintaining a healthy prostate while benefiting from testosterone therapy.
4. Lifestyle, Diet, And Supplements For Prostate Health
The Best Diet For A Healthy Prostate
Diet plays a crucial role in prostate health, influencing inflammation, hormonal balance, and overall well-being. A diet rich in whole, nutrient-dense foods may help reduce the risk of prostate issues, including BPH and prostate cancer.
Foods That Support Prostate Health:
- Cruciferous Vegetables (broccoli, cauliflower, kale) – Contain compounds that may support hormone metabolism.
- Tomatoes – Rich in lycopene, an antioxidant associated with prostate protection.
- Fatty Fish (salmon, mackerel, sardines) – Provide omega-3 fatty acids, which have potential anti-inflammatory properties.
- Nuts and Seeds (walnuts, pumpkin seeds) – Contain healthy fats and minerals beneficial for prostate function.
- Green Tea – Contains polyphenols that may support prostate health.
Foods To Limit Or Avoid:
- Processed Meats – Associated with higher risks of prostate issues.
- Excessive Dairy – Some studies suggest high dairy intake may contribute to prostate inflammation.
- High-Sugar Diets – May lead to insulin resistance, which is linked to metabolic dysfunction and increased prostate enlargement.
Can Certain Foods Reduce Prostate Cancer Risk?

While diet alone is not a cure-all, research suggests that certain foods and dietary patterns may lower prostate cancer risk:
- Mediterranean Diet – Emphasizes anti-inflammatory foods such as olive oil, vegetables, and lean proteins.
- Plant-Based Diets – Some studies suggest reducing red meat and increasing plant-based foods can be beneficial.
- Soy Products – Contain phytoestrogens that may help balance hormonal levels.
Expert insight from Dr. Morgentaler suggests that while diet can play a supportive role in prostate health, hormonal balance remains a more significant factor in managing prostate conditions. He has emphasized that prostate cancer risk is not driven by testosterone levels, and dietary modifications alone are unlikely to outweigh the impact of proper hormone management.
The Impact Of Inflammation On Prostate Health
Chronic inflammation is a major factor in prostate enlargement and irritation. Reducing systemic inflammation through diet, lifestyle, and supplementation may help improve urinary symptoms and long-term prostate health.
Key Anti-Inflammatory Strategies:
- Maintaining a balanced ratio of omega-3 to omega-6 fatty acids.
- Reducing excessive processed food and refined carbohydrate intake.
- Including antioxidant-rich foods such as berries, dark leafy greens, and nuts.
Metabolic Syndrome & Prostate Health: The Overlooked Connection

Metabolic syndrome—a cluster of conditions including obesity, insulin resistance, high blood sugar, and hypertension—is a major but often ignored factor in prostate health. Men with metabolic dysfunction have higher risks of BPH, urinary symptoms, and even aggressive prostate cancer.
How Metabolic Syndrome Affects the Prostate
- Increased Insulin & IGF-1 Promote Prostate Growth
- High insulin levels fuel prostate enlargement (BPH) and may contribute to prostate cancer growth.
- IGF-1 (Insulin-like Growth Factor 1), often elevated in metabolic syndrome, stimulates prostate cell proliferation, increasing risk of cancer.
- Obesity Drives Chronic Inflammation
- Visceral fat produces inflammatory cytokines (IL-6, TNF-alpha), which contribute to prostate inflammation and enlargement.
- Overweight men tend to have higher estrogen levels, which may worsen BPH and urinary symptoms.
- Insulin Resistance & Poor Prostate Outcomes
- Insulin resistance leads to higher fasting glucose levels, which fuel cancer cell metabolism and increase oxidative stress.
- Diabetics have a higher risk of aggressive prostate cancer and worse post-treatment outcomes.
- Testosterone, Metabolic Syndrome & Prostate Function
- Low testosterone is linked to metabolic syndrome, yet many doctors still wrongly assume that TRT worsens prostate health.
- Restoring healthy testosterone levels improves insulin sensitivity, lowers inflammation, and may protect the prostate.
How to Improve Metabolic Health for Prostate Protection
- Reduce processed carbs and sugar to prevent insulin resistance.
- Intermittent fasting and low-carb diets improve insulin function and reduce prostate inflammation.
- Increase activity levels (strength training, walking after meals) to improve glucose metabolism.
- Optimize testosterone levels to support metabolic function and reduce visceral fat.
Supplements That Support Prostate Health

Several supplements have been studied for their potential benefits in prostate health. While not a replacement for proper medical care, they may offer additional support.
- Saw Palmetto – Traditionally used to support urinary function and prostate health. Some studies show benefits, while others remain inconclusive.
- Beta-Sitosterol – A plant sterol that may help reduce urinary symptoms related to BPH.
- Zinc – Plays a role in immune function and hormone balance.
- Magnesium – Some anecdotal reports suggest magnesium supplementation may reduce nocturia (frequent nighttime urination).
- Curcumin (Turmeric Extract) – An anti-inflammatory compound that may support prostate health.
Prostavive is a comprehensive prostate supplement that combines many of the beneficial ingredients mentioned above. It contains zinc and magnesium for hormone balance, plus specialized extracts like Stinging Nettle Root, Tongkat Ali, and Ashwagandha. The formula also includes boron, which research suggests may help maintain healthy hormone levels. Prostavive offers a convenient all-in-one solution for men looking to support optimal prostate function as they age.
Choline, Eggs, And Prostate Cancer – What’s The Truth?

There has been controversy over whether choline (found in eggs, meat, and dairy) is linked to an increased risk of prostate cancer. Some studies suggest a correlation, but others argue this is weak and inconclusive.
- Choline is essential for brain and liver health, making it a necessary nutrient.
- The risk association with prostate cancer remains debated, and it’s unclear if choline itself is problematic or if dietary patterns play a larger role.
- Context matters – Moderation and overall dietary patterns are more significant than demonizing a single nutrient.
Omega-3s And Prostate Health – Do They Help Or Hurt?

Some conflicting studies have questioned whether omega-3 fatty acids influence prostate cancer risk.
- Omega-3s from whole food sources (fish) are generally beneficial for reducing inflammation.
- Fish oil supplements have been inconsistently linked to prostate cancer risk, but no causal relationship has been established.
Expert insights indicate that systemic inflammation is a bigger concern than omega-3 intake itself, and maintaining a diet rich in whole food sources of omega-3s is preferable over reliance on supplementation.
Do High-Fat Diets Increase The Risk Of Prostate Cancer?
High-fat diets, particularly those rich in processed and unhealthy fats, have been associated with increased risks of prostate issues. However, not all fats are equal:
- Healthy Fats (Olive oil, Avocados, Nuts) – Beneficial for hormonal balance and inflammation reduction.
- Unhealthy Fats (Trans fats, Seed oils) – May contribute to metabolic dysfunction and systemic inflammation.
Does Coffee Or Alcohol Affect The Prostate?

- Coffee – Some studies suggest moderate coffee consumption may lower prostate cancer risk, but excessive intake could contribute to bladder irritation.
- Alcohol – Excessive alcohol consumption may contribute to inflammation and disrupt hormone metabolism, potentially impacting prostate health. However, nothing has been definitively found or linked to in the research.
The Role Of Exercise In Preventing Prostate Issues
Regular physical activity is strongly linked to improved prostate health and reduced risks of prostate-related conditions.
- Reduces systemic inflammation and supports metabolic health.
- Improves circulation and urinary function.
- May help regulate hormones related to prostate growth.
Can Losing Weight Improve Prostate Symptoms?

Excess body fat is associated with higher levels of inflammation and hormonal imbalances, which can negatively affect prostate health.
- Losing weight may reduce BPH symptoms.
- Improving insulin sensitivity can help regulate hormonal balance.
Should You Avoid Dairy For Prostate Health?

Some research suggests that high dairy consumption may be associated with increased prostate cancer risk, but findings are mixed. Factors to consider:
- Dairy’s hormonal content (naturally occurring estrogens in milk).
- Individual lactose tolerance and inflammatory response.
- Fermented dairy like kefir may be better than high-fat pasteurised dairy.
Where possible, stick to organic raw unpasteurized dairy that hasn’t been processed by big dairy. Support local organic farmers.
Intermittent Fasting And Prostate Health – Is There A Link?

Intermittent fasting (IF) has been explored as a potential tool for reducing inflammation and improving metabolic health. Some potential benefits include:
- Reduced insulin resistance, which is linked to BPH and prostate cancer.
- Enhanced cellular repair mechanisms.
- Lower levels of systemic inflammation.
The Gut-Prostate Connection: How Your Microbiome Affects Prostate Health

The gut microbiome—the trillions of bacteria in the digestive tract—plays a major role in prostate health. An unhealthy gut microbiome has been linked to increased inflammation, hormonal imbalances, and even higher prostate cancer risk.
How Gut Health Affects the Prostate
- Dysbiosis & Chronic Inflammation
- An imbalance in gut bacteria (dysbiosis) leads to higher systemic inflammation, which may worsen BPH and prostate irritation.
- Inflammatory gut conditions (leaky gut, IBS, Crohn’s disease) have been linked to higher PSA levels.
- The Estrogen-Gut Link
- The gut microbiome regulates estrogen metabolism via the estrobolome, influencing prostate hormone balance.
- Dysbiosis may lead to higher circulating estrogen levels, which can exacerbate BPH and possibly prostate cancer risk.
- Short-Chain Fatty Acids (SCFAs) & Prostate Protection
- Healthy gut bacteria produce SCFAs (butyrate, propionate, acetate), which have anti-inflammatory effects that may protect the prostate.
- Diets low in fiber harm gut bacteria, reducing SCFA production and increasing inflammation.
How to Improve Gut Health for Prostate Protection
- Increase fiber intake (vegetables, resistant starches, fermented foods).
- Avoid excessive antibiotics and processed foods, which disrupt microbiome balance.
- Consume probiotics and prebiotics to support beneficial gut bacteria.
- Manage stress, as chronic stress disrupts the gut-brain axis and worsens inflammation.
Can Anti-Inflammatory Diets Help Prevent Prostate Issues?
- Diets rich in antioxidants, polyphenols, and healthy fats can help reduce inflammation.
- Avoiding excessive processed foods, sugars, and inflammatory fats is key.
Key Takeaways
- Diet plays a significant role in prostate health, with whole foods and balanced nutrition being essential.
- Certain foods like tomatoes, cruciferous vegetables, and fatty fish provide beneficial compounds.
- Supplements like saw palmetto and beta-sitosterol may offer support but are not a replacement for a holistic approach.
- Maintaining a healthy weight, exercising, and reducing systemic inflammation are critical factors in prostate health.
- No single food or supplement will prevent prostate issues—balanced lifestyle choices matter most.
Conclusion
A well-structured diet and healthy lifestyle choices can support prostate health and hormone balance, but they should be part of a broader strategy that includes proper medical oversight, metabolic health, and hormone management. The key to prostate health is a holistic approach that integrates diet, exercise, inflammation control, and personalized medical care.
5. Prostate Health Monitoring And Preventative Care

Should Every Man Over 40 Get A PSA Test? Why The Answer Is More Complicated
The question of whether all men over 40 should undergo routine PSA testing has been widely debated. While early detection of prostate cancer can be beneficial in some cases, PSA testing has also led to significant overdiagnosis and overtreatment. The decision to test should be based on individual risk factors rather than a one-size-fits-all approach.
Key considerations:
- PSA levels can rise for reasons unrelated to cancer, including infections, BPH, or recent sexual activity.
- Routine testing in low-risk men may lead to unnecessary biopsies and anxiety.
- Family history, race, and personal health history should factor into the decision.
Why Routine PSA Testing Can Be Dangerous – A Breakdown From The Great Prostate Hoax
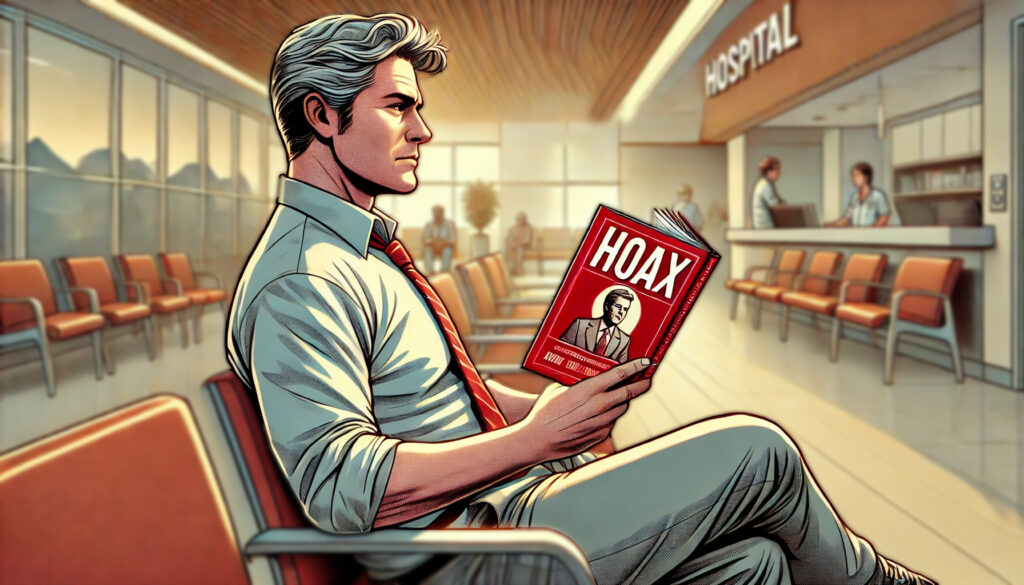
Dr. Richard Ablin, who discovered PSA, has been outspoken about the misuse of PSA testing. His book The Great Prostate Hoax details how PSA screening became a billion-dollar industry despite its poor reliability as a cancer diagnostic tool.
- Many men diagnosed with prostate cancer via PSA testing have low-risk, non-aggressive tumors that would never cause harm.
- Aggressive treatment for these tumors can lead to impotence, incontinence, and reduced quality of life.
- Studies have shown that routine PSA screening does not significantly reduce overall mortality from prostate cancer.
MRI Vs. PSA Testing – Which Is More Accurate?

While PSA testing is often used as an initial screening tool, MRI has emerged as a more accurate and less invasive method for detecting significant prostate cancer.
- PSA limitations: Can be elevated for many reasons beyond cancer, leading to false positives.
- MRI benefits: Can provide a clearer image of suspicious lesions and help avoid unnecessary biopsies.
- Best approach: If PSA is elevated, an MRI should be considered before moving to biopsy.
Natural & Alternative Testing Methods for Prostate Health
Most men rely on PSA tests and biopsies, but alternative testing methods can provide a more comprehensive and less invasive way to monitor prostate health.
Key Alternative Testing Methods
- PHI (Prostate Health Index) & 4Kscore Test
- These tests analyze PSA subtypes to provide a more accurate risk assessment for aggressive prostate cancer.
- PHI combines total PSA, free PSA, and proPSA levels to predict cancer risk better than PSA alone.
- 4Kscore includes additional kallikrein markers to assess whether a biopsy is truly needed.
- PCA3 Urine Test
- PCA3 is a prostate cancer-specific gene test that detects cancer-related RNA in urine.
- Unlike PSA, PCA3 is not influenced by BPH or prostatitis.
- A high PCA3 score may indicate a need for further investigation.
- SelectMDx Urine Test
- A genetic test that predicts the likelihood of aggressive prostate cancer before biopsy.
- Helps reduce unnecessary invasive procedures for men with elevated PSA.
- Liquid Biopsies & Exosome-Based Testing
- Measures tumor-derived DNA, RNA, or proteins in blood or urine to detect aggressive cancers.
- More research is needed, but this could replace traditional biopsies in the future.
Why These Alternatives Matter
- More accurate than PSA alone at identifying aggressive cancer.
- Reduces unnecessary biopsies and overtreatment.
- Non-invasive and safer compared to transrectal prostate biopsies.
When to Consider Alternative Testing
- If PSA is high but MRI is inconclusive.
- If you want a second opinion before agreeing to a biopsy.
- If you are on active surveillance and need better monitoring tools.
Can Early-Stage Prostate Cancer Be Reversed Through Diet And Lifestyle?
Emerging research suggests that intensive lifestyle changes, including dietary modifications, may influence the progression of early-stage, low-grade prostate cancer. A notable study published in the Journal of Urology found that men who adopted a plant-based diet, engaged in regular exercise, and practiced stress management techniques experienced a decrease in prostate-specific antigen (PSA) levels, whereas those who did not make these changes saw an increase in PSA levels.
Further supporting this, a study highlighted by the Prostate Cancer Foundation indicated that among men with more aggressive prostate cancer (Gleason grade 7 or higher), those adhering to a healthful plant-based diet had a 55% lower risk of disease progression compared to those with lower adherence.
While these findings are promising, it’s important to approach them with caution. The relationship between diet, lifestyle, and cancer progression is complex, and individual responses can vary. Therefore, any lifestyle modifications should be discussed with healthcare providers to ensure they complement existing treatment plans and address individual health needs.
Incorporating these insights, men with early-stage prostate cancer might consider adopting a plant-based diet, engaging in regular physical activity, and practicing stress reduction techniques as part of a comprehensive approach to managing their condition.
How To Reduce Your Risk Of Prostate Problems Without Unnecessary PSA Testing

For men who want to monitor prostate health while avoiding unnecessary interventions, several strategies can help reduce risks naturally:
- Focus on metabolic health: Insulin resistance and obesity are linked to higher prostate cancer risk.
- Manage inflammation: A diet rich in antioxidants, healthy fats, and low in processed foods supports overall prostate function.
- Hormone optimization: Maintaining balanced testosterone, DHT, and estrogen levels may reduce prostate enlargement risks.
- Exercise regularly: Reduces inflammation, supports circulation, and helps maintain a healthy weight.
The Role Of Genetics In Prostate Cancer Risk Vs. PSA Testing Failures
While genetics play a role in prostate cancer risk, PSA testing often fails to distinguish between aggressive and indolent tumors. Key points to consider:
- Men with a strong family history of prostate cancer should discuss more advanced screening options beyond PSA.
- Genetic mutations (such as BRCA1/2) can increase risk, making targeted screening more relevant for some individuals.
- Relying solely on PSA testing ignores the complexity of genetic and lifestyle factors that influence prostate health.
Does PSA Screening Lead To Unnecessary Prostate Surgeries?
The aggressive push for PSA screening has led to an increase in unnecessary prostate surgeries, often for low-risk cancers.
- Studies show that many prostate surgeries performed as a result of PSA testing were unnecessary, leading to lifelong side effects like erectile dysfunction and incontinence.
- Active surveillance is often a better approach for men with slow-growing tumors, avoiding unnecessary treatments while keeping an eye on any potential progression.
- MRI and advanced biomarkers can help determine if a prostate tumor truly requires intervention.
Mainstream vs. Expert Advice: What Is The Best Way To Monitor Prostate Health On TRT?
There is a clear divide between mainstream medical guidelines and expert opinions regarding prostate health monitoring for men on TRT.
Mainstream view:
- PSA should be checked regularly, and any increase is considered concerning.
- Many doctors remain cautious about TRT due to outdated beliefs about its relationship to prostate cancer.
Expert perspective:
- A slight PSA increase on TRT is normal and does not indicate cancer.
- More important than PSA alone is the rate of PSA change over time and additional diagnostic tools like MRI when needed.
- Prostate cancer is not fueled by TRT, as supported by modern research and clinical observations.
Key Takeaways
- PSA testing is not always necessary and can lead to overdiagnosis and overtreatment.
- The PSA test was never intended as a universal screening tool, and its misuse has created a public health issue.
- MRI offers a more accurate alternative to PSA for detecting significant prostate cancer.
- Genetics play a role in prostate cancer risk, but lifestyle and metabolic health are also critical factors.
- Active surveillance is often better than immediate treatment for low-risk prostate cancer.
- Men on TRT should not overreact to minor PSA fluctuations, as these do not necessarily indicate cancer.
- Lifestyle and dietary modifications may play a role in slowing or even reversing early-stage prostate cancer progression, but this should always be part of a well-rounded medical approach.
Conclusion
Prostate health monitoring should be personalized, focusing on risk factors, lifestyle modifications, and advanced diagnostics rather than an outdated reliance on PSA testing. While screening is important for some men, routine PSA testing for all men often does more harm than good. Understanding the limitations of PSA and incorporating more precise monitoring tools can help men make better-informed decisions about their prostate health.
6. Medical Treatments And Prostate Health
Gleason Grade and Prostate Cancer Staging: Understanding Your Diagnosis
A prostate cancer diagnosis is not just about “you have cancer” or “you don’t.” The Gleason Score and cancer staging determine how aggressive the cancer is, whether treatment is necessary, and which options are best.
The Gleason Score: What It Means
The Gleason grading system is the most important factor in assessing prostate cancer severity. It evaluates how abnormal prostate cells look under a microscope, assigning two numbers (the primary and secondary Gleason patterns) that add up to the total Gleason Score.
| Gleason Score | Risk Category | What It Means |
| 6 (3+3) | Low-Risk | Slow-growing, unlikely to spread. Often better managed with active surveillance. |
| 7 (3+4 or 4+3) | Intermediate-Risk | Mixed behavior: 3+4 is less aggressive, 4+3 is more concerning. Treatment depends on factors like PSA levels and MRI findings. |
| 8-10 (4+4, 4+5, 5+4, 5+5) | High-Risk | Aggressive cancer, more likely to spread. Active treatment is usually required. |
- A Gleason 6 is NOT a death sentence. Many doctors rush to treat it unnecessarily.
- A Gleason 7 (3+4) behaves more like a 6, while 4+3 behaves more like an 8.
- A Gleason 8-10 needs aggressive management, often surgery or radiation combined with hormone therapy.
Prostate Cancer Staging: How Far Has It Spread?
Beyond Gleason scoring, staging (TNM system) determines how advanced the cancer is:
- T (Tumor Stage) – How big is the tumor?
- T1 – Microscopic, found via biopsy or PSA test (often non-threatening).
- T2 – Confined to the prostate but large enough to be detected by DRE or imaging.
- T3 – Has spread beyond the prostate capsule.
- T4 – Invaded nearby organs (bladder, rectum).
- N (Lymph Node Involvement) – Has it spread to nearby lymph nodes?
- N0 – No lymph node involvement.
- N1 – Cancer has reached nearby lymph nodes.
- M (Metastasis) – Has it spread to distant sites?
- M0 – No distant spread.
- M1 – Cancer has metastasized to bones, liver, lungs, etc.
How Gleason & Staging Guide Treatment Decisions
- Gleason 6 + T1 or T2? → Active surveillance is usually the best option.
- Gleason 7 + localized cancer? → Surgery, radiation, or focal therapy may be needed.
- Gleason 8+ or T3/T4? → Requires aggressive treatment (radiation, hormone therapy, or surgery).
Why This Matters
- Many low-risk men are overtreated because they panic over a cancer diagnosis.
- Many high-risk men are undertreated because their doctor assumes “all prostate cancers are slow-growing.”
- Understanding your Gleason Score and Stage ensures you get the right treatment and avoid unnecessary procedures.
Multiparametric MRI vs. Biopsy: The Smarter Way To Diagnose Prostate Cancer
For decades, prostate biopsies were the standard way to diagnose cancer, but they come with risks, inaccuracies, and unnecessary procedures. Newer multiparametric MRI (mpMRI) scans can often detect clinically significant prostate cancer without an invasive biopsy.
The Problems with Traditional Prostate Biopsies
Most doctors still rely on Transrectal Ultrasound-Guided (TRUS) biopsies, but these have major flaws:
- Random Sampling: Traditional biopsies use a 12-core random needle approach, which misses cancerous areas or detects harmless ones, leading to false negatives or overtreatment.
- High Infection Risk: TRUS biopsies involve inserting needles through the rectal wall, leading to sepsis risks.
- Can Spread Cancer Cells: There’s evidence that biopsies can cause needle tracking, potentially spreading cancerous cells.
- Unnecessary Biopsies: Many biopsies are triggered by an elevated PSA, which may be due to BPH, prostatitis, or other benign causes.
Why Multiparametric MRI (mpMRI) is a Game-Changer
A multiparametric MRI (mpMRI) scan provides detailed, real-time imaging of the prostate, allowing doctors to:
- Detect aggressive cancers more accurately.
- Avoid unnecessary biopsies in men with low-risk findings.
- Use targeted biopsies instead of random ones, reducing the chance of missing a tumor.
Key advantages of MRI over biopsy:
| Factor | Traditional Biopsy | Multiparametric MRI (mpMRI) |
|---|---|---|
| Accuracy | Often misses aggressive cancers | More precise detection |
| Non-Invasive? | No, requires needles in prostate | Yes, no needles required |
| Risk of Infection? | High (sepsis risk) | None |
| Overdiagnosis Risk? | High | Lower |
| Can Guide Targeted Biopsy? | No (random samples) | Yes (exact tumor location) |
Who Should Get an MRI Before a Biopsy?
Men with:
- Elevated PSA but no other risk factors (avoiding unnecessary biopsy).
- Previous negative biopsy but rising PSA (to check if something was missed).
- Known prostate cancer on active surveillance (to monitor without repeat biopsies).
When a Biopsy is Still Needed
- If MRI detects a high-risk lesion, a targeted biopsy can confirm the diagnosis.
- If PSA is persistently rising but MRI is unclear, a fusion biopsy (MRI + ultrasound-guided) is preferred over a traditional biopsy.
Bottom Line: MRI First, Biopsy Only If Necessary
- MRI should be the first-line diagnostic tool for prostate cancer, not immediate biopsy.
- If an MRI shows no clinically significant cancer, a biopsy is often unnecessary.
- If a biopsy is needed, it should be MRI-guided, not random sampling.
Best Medications For Enlarged Prostate (BPH)

Several medications are commonly prescribed to manage BPH symptoms, each targeting different mechanisms to improve urinary function.
- Alpha-Blockers (Tamsulosin, Doxazosin, Terazosin) – Relax prostate and bladder muscles to improve urine flow.
- 5-Alpha Reductase Inhibitors (Finasteride, Dutasteride) – Reduce prostate size by blocking the conversion of testosterone to DHT.
- Combination Therapy (Dutasteride + Tamsulosin) – Some men benefit from using both types of medication together.
- Anticholinergics and Beta-3 Agonists – Used for overactive bladder symptoms related to BPH.
While these medications help with symptoms, they come with potential side effects, including dizziness, sexual dysfunction, and fatigue. Hormonal balance should be considered before using 5-alpha reductase inhibitors, as blocking DHT may negatively impact overall well-being. Some experts advise against using Finasteride altogether due to its negative effects on the body.
What Is The UroLift Procedure, And Does It Work?

UroLift is a minimally invasive procedure designed to relieve BPH symptoms without major surgery. It involves inserting small implants that lift and hold the prostate tissue away from the urethra, reducing urinary obstruction.
Pros:
- Quick recovery time
- No need for cutting or removing prostate tissue
- Preserves sexual function
Cons:
- May not be effective for men with very large prostates
- Some men experience persistent urgency or discomfort post-procedure
Prostate Surgery Options – When Is It Necessary?
Surgery is typically reserved for severe BPH cases or prostate cancer treatment. The most common surgical procedures include:
- Transurethral Resection of the Prostate (TURP) – Removes excess prostate tissue to improve urine flow.
- Holmium Laser Enucleation of the Prostate (HoLEP) – A laser-based alternative to TURP.
- Open Prostatectomy – For extremely enlarged prostates, where a portion of the prostate is surgically removed.
Surgery can effectively relieve symptoms but carries risks such as retrograde ejaculation, incontinence, and erectile dysfunction.
Radiation Therapy Vs. Surgery For Prostate Cancer – Pros And Cons
For men diagnosed with prostate cancer, treatment decisions often come down to surgery or radiation therapy. Each option has advantages and drawbacks.
Radiation Therapy:
- External Beam Radiation (EBRT) – Targets the prostate with high-energy X-rays.
- Brachytherapy – Implants radioactive seeds directly into the prostate.
Pros:
- Non-invasive, no hospital stay required
- Lower risk of immediate urinary incontinence
Cons:
- Can cause bowel and bladder irritation
- Delayed onset of side effects (may appear years later)
Prostatectomy (Surgical Removal of the Prostate):
- Radical Prostatectomy – Complete removal of the prostate, often used for aggressive cancers.
Pros:
- Immediate removal of cancerous tissue
- PSA levels drop to near zero, allowing better monitoring
Cons:
- Higher risk of erectile dysfunction and urinary incontinence
- Requires a longer recovery period
The choice between surgery and radiation depends on cancer aggressiveness, patient age, and personal preferences.
Alternative Therapies For Prostate Cancer And BPH
For men seeking less invasive or non-toxic alternatives to traditional treatments, several options exist that offer promising results without the severe side effects associated with radiation or chemotherapy.
Cryotherapy
Cryotherapy, or cryosurgery, is a treatment that freezes and destroys prostate cancer cells using extremely cold temperatures. This technique can be effective for localized prostate cancer while preserving surrounding healthy tissue.
Pros:
- Minimally invasive with a quick recovery
- Can be repeated if necessary
- Lower risk of long-term incontinence compared to surgery
Cons:
- Can cause temporary swelling or discomfort
- May not be suitable for larger or more aggressive tumors
Proton Therapy
Proton beam therapy is a targeted form of radiation that delivers high-energy protons directly to the tumor, reducing damage to surrounding tissues.
Pros:
- More precise than traditional radiation therapy
- Less risk of bowel and bladder irritation
Cons:
- Limited availability and higher cost
- Long-term data is still being studied
Focal Therapy
Focal therapy targets only the cancerous areas of the prostate while preserving the rest of the gland. This is an emerging option for men with small, localized tumors.
Pros:
- Minimally invasive, preserving prostate function
- Fewer side effects than surgery or radiation
Cons:
- Requires advanced imaging for accurate targeting
- Not widely available yet
Stereotactic Body Radiation Therapy (SBRT)
SBRT is a high-dose, targeted radiation treatment that delivers precise beams of radiation over a shorter period than conventional radiation therapy.
Pros:
- Shorter treatment duration (1-5 sessions vs. weeks of conventional radiation)
- More precise targeting reduces collateral damage
Cons:
- Potential for localized irritation (bladder or rectum)
- Still considered a newer treatment with ongoing research
Radiofrequency Ablation (RFA)
Radiofrequency ablation uses high-frequency electrical currents to destroy abnormal prostate tissue. This therapy is being explored for both BPH and prostate cancer.
Pros:
- Minimally invasive with minimal downtime
- Can be repeated as needed
Cons:
- Limited long-term studies
- Not widely available yet
Can Hormone Therapy Help Manage Prostate Cancer?
Androgen deprivation therapy (ADT) is sometimes used to slow the progression of prostate cancer by lowering testosterone levels.
- Medications (Leuprolide, Degarelix) – Suppress testosterone production.
- Anti-Androgens (Bicalutamide, Enzalutamide) – Block androgen receptors to limit cancer growth.
- Orchiectomy (Surgical Castration) – A permanent method to eliminate testosterone production.
While ADT can slow cancer progression, long-term use can lead to osteoporosis, muscle loss, fatigue, and cardiovascular risks.
Testosterone And Prostate Surgery – What To Know
For men who have undergone prostate surgery, particularly radical prostatectomy, questions about TRT often arise.
- Traditional medical guidance discourages TRT post-surgery due to fears of cancer recurrence.
- Newer research suggests that TRT may be safe for men who have undergone prostate removal with no evidence of disease.
- Close monitoring is essential if TRT is restarted post-surgery.
Are There TRT Protocols For Men With A History Of Prostate Cancer?
Many doctors are hesitant to prescribe TRT to men with a history of prostate cancer, but modern research challenges the outdated notion that testosterone fuels prostate cancer.
- Men with a history of low-risk prostate cancer who have been cancer-free for years may be candidates for TRT.
- Some physicians use a cautious approach, starting with low-dose TRT and monitoring PSA levels closely.
- Studies indicate that restoring normal testosterone levels may improve quality of life without increasing cancer recurrence risk.
Can TRT Be Used Safely After Prostate Cancer Treatment?
Recent evidence suggests that TRT can be used cautiously after prostate cancer treatment, particularly in men with non-aggressive cancers who have undergone successful treatment.
- Men who underwent radical prostatectomy with undetectable PSA levels are often the best candidates.
- Active surveillance is key – PSA levels should be monitored regularly to ensure no recurrence.
- Symptoms of low testosterone should not be ignored, as hormone deficiency can negatively impact metabolic health, bone density, and quality of life.
TRT, PSA Monitoring, And Patient Experiences
Anecdotal reports from TRT users suggest that some men see temporary PSA fluctuations after starting TRT, which can cause concern but is often not indicative of cancer progression. Some men undergoing post-cancer TRT report that PSA levels stabilized over time, while others had to adjust dosages based on PSA responses.
A discussion from TRT community members highlighted cases where doctors unfamiliar with testosterone therapy misinterpreted PSA rises, leading to unnecessary biopsies. This underscores the importance of working with providers experienced in hormone therapy and prostate health.
New Treatments For BPH And Prostate Cancer – What’s On The Horizon?

Innovative treatments are emerging to offer less invasive and more targeted therapies for both BPH and prostate cancer.
- High-Intensity Focused Ultrasound (HIFU) – Uses ultrasound waves to destroy cancerous tissue without surgery.
- Prostatic Artery Embolization (PAE) – A non-surgical procedure that shrinks the prostate by reducing blood supply.
- Immunotherapy & Targeted Therapies – Emerging cancer treatments that leverage the immune system to attack tumors more precisely.
Key Takeaways
- Medications like alpha-blockers and 5-ARIs can help with BPH symptoms but have side effects.
- UroLift and other minimally invasive procedures offer alternatives to surgery for BPH relief.
- Radiation and surgery are primary treatment options for prostate cancer, each with pros and cons.
- Hormone therapy is used for advanced prostate cancer but comes with significant risks.
- New research supports the safe use of TRT in some men with a history of prostate cancer.
- Emerging treatments like HIFU and immunotherapy may improve outcomes with fewer side effects.
Conclusion
Medical treatments for prostate conditions range from medications to surgical interventions, with new therapies continually emerging. While traditional approaches remain effective, modern research challenges outdated fears about testosterone therapy and prostate cancer. Men should work closely with their doctors to evaluate their options and determine the best course of action based on their individual risk factors and health goals.
7. Misconceptions And Myths About Prostate Health
The PSA Test Was Not Designed To Diagnose Prostate Cancer – How It Was Hijacked By Big Medicine
The PSA test was originally developed as a tool to monitor prostate cancer progression in men who had already been diagnosed, not as a general screening test. However, it was later pushed as a universal screening tool, leading to unnecessary anxiety, biopsies, and even overtreatment.
- False Positives – PSA levels can rise due to infections, BPH, or even recent sexual activity, leading to unnecessary biopsies.
- Overdiagnosis – Many men diagnosed with prostate cancer via PSA testing have slow-growing tumors that would never cause harm.
- Financial Incentives – The widespread use of PSA testing has benefited the medical industry financially, even though it has led to unnecessary treatments for many men.
Does High PSA Always Mean Cancer? Why Millions Of Men Have Been Misled
One of the biggest misconceptions is that an elevated PSA automatically signals prostate cancer. In reality, PSA levels can be influenced by multiple factors:
- BPH (Benign Prostatic Hyperplasia) – A common condition in aging men that increases PSA levels but is not cancerous.
- Prostatitis (Prostate Inflammation) – Temporary PSA spikes due to infection or inflammation.
- Age-Related Increase – PSA naturally rises with age, making blanket cutoffs problematic.
Are Men On TRT More Likely To Get High PSA Readings? Understanding The Science
Many doctors remain hesitant about prescribing TRT to men due to outdated fears about PSA increases and prostate cancer risk. However, modern research has found:
- TRT does not increase prostate cancer risk – No credible studies have shown that properly managed TRT leads to higher rates of prostate cancer.
- Mild PSA increases are common but not dangerous – Some men experience a slight rise in PSA after starting TRT, but this stabilizes over time.
- PSA velocity matters more than a single reading – A sudden, sharp rise in PSA is more concerning than a gradual increase over time.
Why Many Men Undergo Unnecessary Prostate Biopsies – A Breakdown Of PSA Misinformation
Due to an overreliance on PSA testing, countless men have undergone unnecessary prostate biopsies, which come with risks such as infection, bleeding, and even erectile dysfunction.
- Biopsies are often performed without considering other diagnostic tools like MRI or free-to-total PSA ratio, which can provide more clarity.
- Many prostate cancers are slow-growing and do not require immediate intervention – Active surveillance is often the best approach.
- Some doctors recommend biopsies too aggressively due to outdated screening protocols.
Other Common Myths And Misconceptions

Additional myths were identified In TRT forums and discussion groups that are widely believed but lack scientific backing.
1. “Finasteride And Dutasteride Are Completely Safe For Prostate Health”
While 5-alpha reductase inhibitors like finasteride and dutasteride are commonly prescribed for BPH, many men report significant side effects, including:
- Reduced libido and erectile dysfunction – Even after stopping the medication (post-finasteride syndrome).
- Cognitive and mood issues – Some users report brain fog and depression.
- Masked PSA Readings – These drugs artificially lower PSA, making it harder to detect prostate cancer early.
2. “Cycling Can Cause Prostate Cancer”
There is a long-standing myth that cycling increases prostate cancer risk due to prolonged pressure on the perineum. However, research shows:
- Cycling does not cause prostate cancer – No strong evidence links cycling to increased cancer risk.
- It may cause temporary PSA spikes – Long rides can elevate PSA levels, but these usually return to normal within a few days.
- Proper bike fit can reduce prostate irritation – Using a well-fitted saddle can prevent unnecessary pressure on the prostate.
3. “A High-Protein Diet Worsens Prostate Cancer”

There is ongoing debate about diet and its impact on prostate cancer, with some claiming that high-protein diets fuel cancer growth. The truth is more nuanced:
- No direct link between high-protein intake and prostate cancer progression has been established.
- Processed meats and excessive dairy may contribute to inflammation, but lean protein sources (fish, poultry, plant-based proteins) are not harmful.
- Overall diet quality matters more than any single macronutrient.
4. “Minoxidil And DHT Blockers Can’t Affect Prostate Health”
Men using minoxidil (for hair loss) or DHT blockers often believe these medications have no effect on prostate health. However:
- DHT plays a role in prostate health – Lowering DHT through medications like finasteride may impact prostate size and function.
- Some men on minoxidil report changes in urinary function – Though rare, anecdotal evidence suggests sensitivity to these medications can impact prostate symptoms.
Key Takeaways
- The PSA test was never intended for general cancer screening and has led to widespread overtreatment.
- A high PSA does not always mean prostate cancer – other factors must be considered.
- TRT does not increase prostate cancer risk, and PSA changes on TRT should be interpreted carefully.
- Many prostate biopsies are unnecessary and alternative diagnostic tools should be used first.
- Common myths around finasteride, cycling, protein intake, and DHT blockers need further scrutiny – the science does not always match mainstream medical advice.
Conclusion
The conversation around prostate health is filled with misinformation that has led to unnecessary fear, aggressive treatments, and outdated medical practices. Understanding the true risks and benefits of PSA testing, TRT, medications, and lifestyle factors is essential for making informed decisions about prostate health. Men should approach these topics with a critical mind, seek multiple perspectives, and avoid fear-driven medical decisions.
Final Thoughts
How To Take Control Of Your Prostate Health Without Falling For PSA Misinformation
The widespread use of PSA testing has led to decades of unnecessary fear, overdiagnosis, and overtreatment. Understanding the limitations of PSA testing and taking a proactive, informed approach to prostate health can prevent men from making reactive decisions based on misleading data.
Key actions to take control:
- Do not rely solely on PSA levels. Use additional diagnostic tools such as multiparametric MRI, PSA velocity analysis, and free-to-total PSA ratio before agreeing to a biopsy.
- Maintain a balanced lifestyle. Diet, exercise, and hormone optimization all play major roles in prostate health and should not be ignored.
- Seek expert opinions. Many doctors still operate on outdated guidelines. Consult urologists or endocrinologists familiar with modern research before making major health decisions.
Key Takeaways From The Great Prostate Hoax On The PSA Testing Epidemic
Dr. Richard Ablin’s book The Great Prostate Hoax exposed how the PSA test was never intended to be a routine screening tool yet was promoted for financial gain, leading to millions of unnecessary treatments.
Main takeaways:
- The PSA test was originally meant to monitor prostate cancer progression, not diagnose it.
- Routine PSA screening leads to false positives, causing fear and unnecessary procedures.
- Many men diagnosed with prostate cancer through PSA testing have low-risk tumors that never needed treatment.
- The medical industry has benefited financially from overtreatment and unnecessary surgeries, often at the expense of men’s quality of life.
What To Discuss With Your Doctor About PSA, TRT, And Prostate Health
When discussing PSA levels, TRT, or prostate health with your doctor, it’s crucial to ask the right questions to avoid unnecessary interventions and misinformation.
Key discussion points:
- “If my PSA is elevated, what other tests can we do before considering a biopsy?”
- “What factors besides cancer could be causing my PSA increase?”
- “Do you follow the latest research on TRT and prostate health?”
- “Can we use MRI or other imaging methods before deciding on invasive procedures?”
- “What is the risk of overtreatment, and can we consider active surveillance first?”
By taking an active role in your health discussions, you can make informed decisions based on scientific evidence rather than outdated protocols.
Resources And Further Reading (Studies, Expert Opinions, And More)
For those looking to further explore prostate health, PSA testing, and TRT, here are some valuable resources:
- Books:
- The Great Prostate Hoax – Dr. Richard Ablin
- Testosterone For Life – Dr. Abraham Morgentaler
- Research Papers & Studies:
- The Saturation Model And Prostate Cancer (Morgentaler et al.)
- Overdiagnosis And Overtreatment Of Prostate Cancer (New England Journal of Medicine)
- TRT And Prostate Cancer Risk: A Meta-Analysis (European Urology)
- Expert Websites:
- Prostate Cancer Foundation (www.pcf.org)
- Urology Care Foundation (www.urologyhealth.org)
Final Word
Prostate health is not just about PSA numbers—it’s about understanding your body, making informed choices, and rejecting outdated medical myths. By combining modern diagnostics, lifestyle changes, and a balanced approach to hormone health, men can take control of their prostate health without falling victim to unnecessary fear and overtreatment. Always challenge misleading mainstream narratives and seek evidence-based medical advice to make the best decisions for your health.
