The Ultimate Guide To Hematocrit On TRT
Last Updated On March 29, 2025
Contents
- Chapter 1: Introduction – Understanding Hematocrit And TRT
- Chapter 2: What Causes Hematocrit To Increase On TRT?
- Chapter 3: The Myths And Misconceptions About High Hematocrit
- Chapter 4: How To Properly Monitor Hematocrit On TRT
- Chapter 5: The Real Hematocrit “Danger Zone” – When Should You Be Concerned?
- Chapter 6: How To Manage High Hematocrit Without Donating Blood
- Chapter 7: Blood Donation – When It’s Necessary and When It’s Not
- Chapter 8: Finding a Doctor Who Understands Hematocrit and TRT
- Chapter 9: Frequently Asked Questions (FAQ)
- Chapter 10: Conclusion – Understanding Hematocrit in the Big Picture
Chapter 1: Introduction – Understanding Hematocrit And TRT
When starting Testosterone Replacement Therapy (TRT), one of the first things you’ll hear about is hematocrit levels. Some doctors closely monitor hematocrit and panic if it rises, while others ignore it unless symptoms appear. The confusion surrounding hematocrit often leads to unnecessary worry, unnecessary blood donations, and even doctors withholding prescriptions over a number on a lab report.
This guide will clear up the confusion. You’ll learn what hematocrit is, why it increases on TRT, when it actually becomes a problem, and how to manage it effectively without unnecessary interventions.
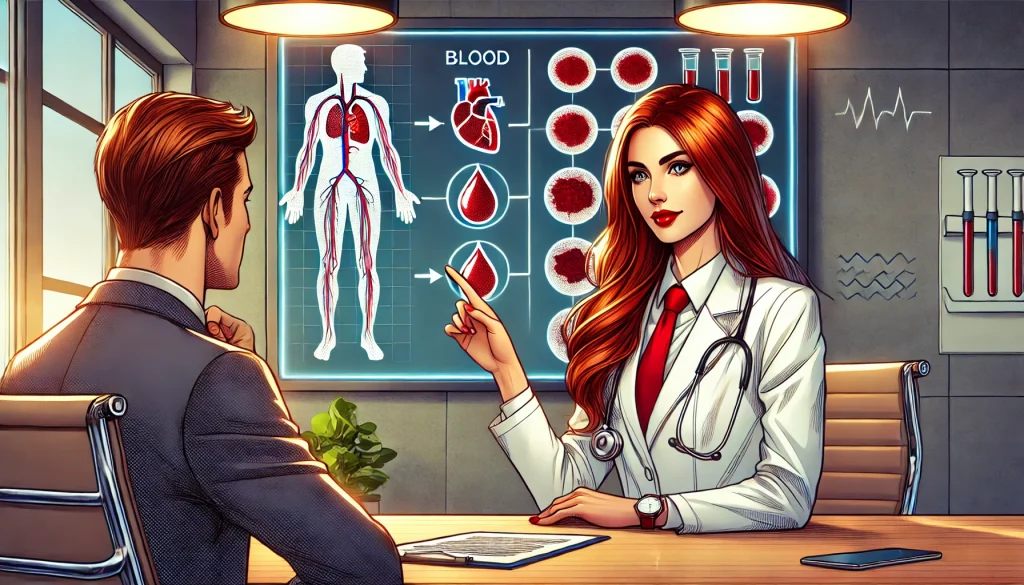
What Is Hematocrit?
Hematocrit (HCT) is the percentage of red blood cells (RBCs) in your blood volume. It’s an essential marker because red blood cells transport oxygen throughout the body. If hematocrit is too low, oxygen delivery suffers, leading to fatigue, weakness, and poor endurance. If it’s too high, blood viscosity increases, which some doctors fear could raise the risk of clotting or cardiovascular issues.
Hematocrit Reference Ranges
- Normal hematocrit levels for men: 38.3% to 52%
- TRT and high-altitude populations often see levels between 52% and 57%
- The TRT “high zone” is typically considered 54-57%, but this does not automatically mean danger
Most labs report hematocrit as a percentage (%), but it can also be presented as a fraction (e.g., 0.52 instead of 52%).
Why Does TRT Increase Hematocrit?
TRT stimulates red blood cell production through increased erythropoiesis, the process by which the body makes new RBCs. This happens primarily through testosterone’s interaction with the kidneys, which produce erythropoietin (EPO)—a hormone that signals the bone marrow to produce more RBCs.
This effect isn’t unique to TRT. Other factors that naturally raise hematocrit include:
- Living at high altitudes (where lower oxygen levels stimulate RBC production)
- Dehydration (which artificially raises hematocrit in blood tests)
- Smoking (which reduces oxygen delivery, prompting the body to compensate)
Most TRT users will see some increase in hematocrit, but this is often harmless unless symptoms appear.
Why Some Doctors Overreact To High Hematocrit
Many doctors mistakenly equate TRT-induced erythrocytosis with polycythemia vera, a rare blood disorder that causes uncontrolled red blood cell production. This misunderstanding leads to:
- Unnecessary blood donations
- Lowering testosterone doses unnecessarily
- Withholding TRT altogether
The key difference? Polycythemia vera is a disease, while TRT-induced erythrocytosis is a natural response to higher testosterone levels.
What You’ll Learn In This Guide
This guide will cover:
- The difference between high hematocrit and real health risks
- When hematocrit actually becomes a concern
- The best ways to manage hematocrit without unnecessary interventions
- Why blood donation is usually not the right solution
- The latest expert insights on hematocrit and TRT
By the end of this guide, you’ll have a clear, practical understanding of hematocrit on TRT—without the misinformation and fear-mongering that surrounds this topic. Let’s get started.
Chapter 2: What Causes Hematocrit To Increase On TRT?

One of the most common lab changes people experience on TRT is an increase in hematocrit. While this is a natural physiological response to testosterone, many TRT users and doctors overreact to the change, often misunderstanding its causes and implications. In this chapter, we will break down the reasons behind hematocrit elevation and how it fits into the bigger picture of TRT management.
Testosterone And Erythropoiesis – How TRT Stimulates Red Blood Cell Production
Testosterone plays a crucial role in the production of red blood cells (RBCs) through a process called erythropoiesis. This occurs primarily due to testosterone’s influence on the kidneys, which stimulates the production of erythropoietin (EPO), a hormone responsible for signaling the bone marrow to produce more RBCs.
When RBC production increases, hematocrit levels rise because hematocrit is simply the percentage of total blood volume made up of RBCs. This is why TRT users commonly see hematocrit levels climb after starting therapy.
Factors That Influence Hematocrit Increase On TRT

While TRT itself is the primary driver of hematocrit elevation, other contributing factors can affect how much an individual’s hematocrit rises:
- Testosterone Dose And Frequency – Higher doses and less frequent injections tend to cause more fluctuations in RBC production, leading to larger spikes in hematocrit.
- Individual Genetics – Some people naturally produce more RBCs in response to testosterone due to genetic differences in erythropoietin sensitivity.
- Hydration Status – Dehydration can artificially inflate hematocrit levels, making them appear higher than they actually are.
- Altitude – People living at higher elevations naturally have higher hematocrit levels due to the lower oxygen environment, which stimulates RBC production.
- Oxygen Demand – Athletes or individuals engaging in high-intensity training may see a greater increase in hematocrit due to the body’s need for improved oxygen transport.
- Smoking And Sleep Apnea – Both conditions reduce oxygen levels in the blood, prompting the body to produce more RBCs to compensate, further increasing hematocrit.
Why Hematocrit Rises More With Injections Compared To Other Delivery Methods
Not all TRT delivery methods affect hematocrit the same way. Intramuscular (IM) injections tend to cause a more pronounced increase in hematocrit compared to topical or subcutaneous (SQ) administration. This is because injections create sharp spikes in testosterone levels, leading to a more significant erythropoietic response.
- Injectable TRT (IM or SQ) – More pronounced increase in hematocrit due to peak testosterone levels following injections.
- Transdermal (Gels, Creams) – Generally causes a lower rise in hematocrit due to steadier, lower testosterone absorption.
- Oral TRT (Undecanoate Capsules) – Can have varied effects on hematocrit, depending on the dosing regimen and absorption rate.
Is A Rise In Hematocrit Always A Bad Thing?
Many doctors and TRT users assume that any increase in hematocrit is automatically harmful. However, this is not necessarily the case. Higher hematocrit does not inherently mean increased clotting risk or cardiovascular danger. Instead, it depends on whether symptoms arise and other blood markers such as platelet count and blood viscosity.
The key takeaway is that hematocrit naturally increases on TRT, but this does not automatically mean intervention is required. Understanding the causes and context behind hematocrit elevation is crucial to making informed decisions regarding TRT management.
In the next chapter, we will address the most common myths and misconceptions surrounding hematocrit on TRT and separate fact from fear-mongering.
When TRT Increases Hematocrit for the Better
While some TRT users are concerned about hematocrit rising too high, there’s another side to the story—for some men, this rise is actually beneficial.
Testosterone plays a key role in red blood cell production, and research has shown that men with low testosterone are significantly more likely to suffer from anemia. Studies have found that TRT corrects low hemoglobin and hematocrit levels, particularly in men with chronic conditions like kidney disease, where low testosterone contributes to poor red blood cell production.
This means that in some cases, TRT does not just raise hematocrit—it restores it to where it should be. Instead of being a risk, it’s a fix for an underlying deficiency. Of course, proper monitoring is still essential, but it’s important to recognize that TRT’s effects on hematocrit are not always negative.
PRO Tip: For a deeper look at how TRT can help with anemia, see our article Anemia in Men: Could Low Testosterone Be the Hidden Cause?
Chapter 3: The Myths And Misconceptions About High Hematocrit

Hematocrit is one of the most misunderstood markers in TRT. Many TRT users and even medical professionals assume that any rise in hematocrit is dangerous and requires immediate intervention. However, much of this concern is based on outdated or misinterpreted data. In this chapter, we will debunk the most common myths about hematocrit on TRT and clarify what the actual risks are.
Myth #1: TRT-Induced Erythrocytosis Is The Same As Polycythemia Vera
One of the biggest misconceptions is that an increase in hematocrit on TRT is the same as polycythemia vera (PV)—a rare blood disorder where the bone marrow produces too many red blood cells uncontrollably.
The key difference is that TRT-induced erythrocytosis is a controlled physiological response to increased testosterone levels, not a disease process. Unlike PV, TRT-induced erythrocytosis does not lead to an increased risk of spontaneous blood clots or uncontrolled RBC production.
Myth #2: High Hematocrit Automatically Means High Blood Viscosity
Many people assume that as hematocrit rises, blood viscosity (thickness) automatically increases to dangerous levels. However, this is an oversimplification.
Blood viscosity is influenced by multiple factors, including:
- Plasma volume and hydration status
- Platelet count and function
- Fibrinogen and other clotting factors
Studies have shown that even at hematocrit levels of 54-57%, blood viscosity does not necessarily reach dangerous levels. Hydration plays a significant role in blood viscosity, and many cases of high hematocrit are simply due to dehydration rather than an actual increase in RBC mass.
Myth #3: High Hematocrit Always Increases Clotting Risk
A common fear is that high hematocrit directly leads to an increased risk of stroke, deep vein thrombosis (DVT), or other clotting disorders. However, research does not support this claim for TRT users without additional risk factors.
Clotting risk is more closely tied to platelet function and overall coagulation markers rather than hematocrit alone. Many individuals, such as those living at high altitudes, naturally have hematocrit levels above 55% without an increased incidence of clotting disorders.
Myth #4: Blood Donation Is Always Necessary For High Hematocrit
Many TRT users are advised to donate blood regularly once their hematocrit reaches 52-54%. However, this is often unnecessary and can lead to unintended consequences like iron depletion, low ferritin, and chronic fatigue.
Instead of rushing to donate blood, TRT users should consider:
- Increasing injection frequency to stabilize testosterone levels
- Ensuring adequate hydration before blood tests
- Evaluating platelet count and blood viscosity markers
If no symptoms are present and clotting markers are normal, there is often no need to donate blood at all.
Myth #5: There Is A Universal “Safe” Hematocrit Threshold
Many doctors and TRT users believe that hematocrit over 52% or 54% is always dangerous, but this is not supported by real-world data. There is no single hematocrit number that defines risk—context matters.
Factors such as:
- Individual oxygen demand
- Cardiovascular health
- Hydration and plasma volume
- Clotting factor levels
… all play a larger role in risk assessment than hematocrit alone.
Takeaways: Facts vs. Fear-Mongering
- TRT-induced erythrocytosis is not a disease and is distinct from polycythemia vera.
- Hematocrit alone does not dictate blood viscosity—hydration and other factors matter.
- Clotting risk is linked more to platelet function and overall coagulation markers than hematocrit itself.
- Blood donation is often unnecessary and can cause more harm than good if done without justification.
- There is no universal hematocrit danger threshold—each case should be assessed individually.
Understanding the truth behind these myths allows TRT users to make informed decisions rather than being misled by outdated or fear-based medical advice. In the next chapter, we will cover how to properly monitor hematocrit levels and interpret test results accurately.
Chapter 4: How To Properly Monitor Hematocrit On TRT

Monitoring hematocrit correctly is essential for understanding its role in TRT and avoiding unnecessary interventions. Many TRT users and even doctors react to a single hematocrit reading without considering context, leading to overcorrections and unnecessary blood donations. In this chapter, we’ll cover how hematocrit is measured, how to prepare for blood tests, and what additional markers should be considered alongside hematocrit.
How Hematocrit Is Measured
Hematocrit is typically measured as part of a Complete Blood Count (CBC) test. It represents the percentage of total blood volume made up of red blood cells.
Units Used For Hematocrit
- Expressed as a percentage (e.g., 50% means half of your blood volume is RBCs)
- Can also be written as a decimal fraction (e.g., 0.50 instead of 50%)
Hematocrit results should always be interpreted in context, alongside other markers like hemoglobin and RBC count.
How To Prepare For A Hematocrit Blood Test
Many TRT users see false elevations in hematocrit due to dehydration, improper test timing, or lifestyle factors. To get an accurate reading:
- Hydrate well before the test – Dehydration can concentrate the blood and artificially raise hematocrit levels.
- Avoid intense exercise before testing – Heavy lifting and endurance exercise can temporarily elevate RBCs.
- Schedule morning tests when possible – Hematocrit can fluctuate throughout the day.
- Minimize caffeine and alcohol intake the day before – Both can affect blood volume and hydration levels.
Hematocrit Vs. Other Blood Markers
Hematocrit alone doesn’t provide the full picture of blood health. It should always be evaluated alongside:
- Hemoglobin – High hemoglobin with high hematocrit suggests increased oxygen-carrying capacity, not necessarily a risk.
- Red Blood Cell (RBC) Count – Elevated RBCs with high hematocrit further confirms erythropoiesis stimulation.
- Platelet Count – If platelets remain normal, clotting risk is lower, even with high hematocrit.
- Blood Viscosity Markers – Fibrinogen, ESR, and CRP levels help assess overall blood thickness.
- Ferritin and Iron Levels – Important for evaluating whether frequent blood donation has led to iron deficiency.
How Often Should You Check Hematocrit?
For TRT users, hematocrit should be monitored at reasonable intervals:
- Every 3-6 months when starting TRT or adjusting dosage.
- Every 6-12 months for stable TRT users with no hematocrit concerns.
- More frequently if previous tests showed significant increases.
Doctors who demand excessive testing without reason may be overreacting. Unless symptoms are present, slight hematocrit increases should not be cause for alarm.
Key Takeaways
- Hematocrit is best assessed alongside hemoglobin, RBC count, and platelet function.
- Proper hydration and test timing help avoid misleading hematocrit readings.
- Routine monitoring is important, but excessive testing is unnecessary unless symptoms arise.
Understanding how to correctly monitor hematocrit ensures you make informed decisions about your TRT protocol. In the next chapter, we’ll explore when hematocrit actually becomes a concern and when intervention may be necessary.
Chapter 5: The Real Hematocrit “Danger Zone” – When Should You Be Concerned?
Many TRT users worry about high hematocrit levels, often due to misleading information from doctors or outdated medical guidelines. While it’s true that extreme elevations in hematocrit can pose risks, the threshold for concern is often misunderstood. In this chapter, we’ll explore when hematocrit actually becomes a problem, what symptoms to watch for, and how to differentiate between benign increases and true medical concerns.
What Hematocrit Level Is “Too High” On TRT?
The common misconception is that hematocrit above 52% or 54% is dangerous, leading many doctors to recommend immediate blood donation or reductions in TRT dosage. However, real-world evidence and expert opinions suggest that the actual concern threshold is 54-57%, and even then, context matters.
Key Factors To Consider With High Hematocrit
Instead of focusing only on the percentage, the following factors should be evaluated:
- Symptoms – High hematocrit is only concerning if accompanied by symptoms like headaches, dizziness, or shortness of breath.
- Blood Viscosity – Hematocrit alone does not determine blood thickness; hydration and other clotting factors play a role.
- Platelet Count – If platelet levels remain normal, clotting risk is lower even with a higher hematocrit.
- Oxygen Saturation Levels – Individuals at high altitudes naturally have hematocrit above 55% with no issues due to increased oxygen demand.
- Blood Pressure – Persistent high blood pressure alongside elevated hematocrit may indicate a need for adjustment.
Symptoms Of Excessive Blood Thickness (When To Take Action)
If hematocrit increases significantly and leads to symptoms, it’s important to assess whether intervention is needed. Some signs to watch for include:
- Persistent headaches
- Dizziness or lightheadedness
- Unexplained shortness of breath
- Blurry vision
- High blood pressure that doesn’t respond to treatment
- Red or flushed skin (often in the face)
If any of these symptoms occur alongside hematocrit above 57%, it may be time to discuss management strategies.
Why Arbitrary Cutoffs Can Be Misleading
The medical field often relies on arbitrary cutoff values rather than assessing the individual patient. Many doctors use outdated thresholds, assuming that once hematocrit hits 52% or 54%, intervention is necessary. However, this blanket approach does not account for:
- Hydration status – Dehydration can temporarily raise hematocrit.
- Testosterone dose and injection frequency – More stable protocols often result in more stable hematocrit levels.
- Individual adaptation – Some people naturally maintain higher hematocrit without issues.
Expert Opinions On When To Be Concerned
Leading TRT experts suggest that symptoms should always be the primary deciding factor, not a number on a lab test. According to their insights:
- Hematocrit between 54-57% is not an automatic problem unless symptoms are present.
- Hydration, platelet count, and overall cardiovascular health must be assessed before taking action.
- Regular blood donations are not needed for most TRT users and can lead to iron depletion and fatigue.
Final Takeaways: Context Over Panic
- Hematocrit above 54% is not automatically dangerous – symptoms and other factors matter.
- Doctors relying solely on hematocrit levels to determine risk are often using outdated guidelines.
- Hydration, platelet count, and blood viscosity should always be considered before taking action.
- If symptoms like dizziness, high blood pressure, or shortness of breath occur with hematocrit above 57%, intervention may be needed.
Understanding when hematocrit is truly a concern will prevent unnecessary worry and poor medical decisions. In the next chapter, we’ll discuss effective strategies for managing hematocrit without relying on frequent blood donations.
Chapter 6: How To Manage High Hematocrit Without Donating Blood

Many TRT users assume that blood donation is the only way to manage high hematocrit, but this is not always necessary—or even the best approach. While bloodletting can temporarily lower hematocrit, it often leads to iron depletion, low ferritin levels, and fatigue, creating more problems than it solves. In this chapter, we’ll explore the most effective ways to manage hematocrit without relying on blood donation.
Why You Should Avoid Unnecessary Blood Donations
Blood donation can be a quick fix for elevated hematocrit, but frequent donations can have unintended consequences:
- Iron depletion – Regular blood loss can strip the body of essential iron, leading to chronic fatigue and poor oxygen transport.
- Lower ferritin levels – Ferritin is the body’s iron storage, and frequent donation can deplete it to dangerously low levels.
- Hematocrit rebound – Many TRT users find that hematocrit rebounds within weeks after donation, leading to a cycle of frequent donations.
- Not addressing the root cause – Instead of temporarily lowering hematocrit, it’s better to focus on long-term solutions that stabilize levels naturally.
Alternative Strategies To Lower Hematocrit Naturally
Instead of donating blood, consider these methods to stabilize hematocrit levels safely:
1. Increase Injection Frequency
Larger, less frequent doses of testosterone cause higher peaks and deeper troughs, which stimulate more erythropoiesis (red blood cell production). By switching to smaller, more frequent injections (e.g., daily or every other day), testosterone levels remain more stable, reducing the excessive stimulation of red blood cell production.
2. Stay Hydrated
Dehydration concentrates the blood, making hematocrit appear higher than it actually is. Proper hydration can naturally lower hematocrit by expanding blood plasma volume.
- Drink plenty of water throughout the day.
- Monitor caffeine and alcohol intake, as both can contribute to dehydration.
- Consider adding electrolytes to maintain proper hydration balance.
3. Incorporate Light Cardio
Aerobic exercise helps regulate hematocrit levels by improving blood circulation and plasma volume.
- Moderate-intensity cardio (30-45 minutes, 3-5x per week) can help balance hematocrit without reducing testosterone benefits.
- Activities such as jogging, cycling, swimming, or brisk walking are effective.
4. Reduce Excess Iron Intake
Iron plays a role in RBC production, and excess dietary iron can contribute to higher hematocrit levels. If hematocrit is creeping too high, consider:
- Avoiding iron supplements unless medically necessary.
- Reducing red meat intake (particularly liver and other organ meats, which are high in iron).
- Checking ferritin and iron levels before assuming donation is needed.
5. Consider Natural Blood Thinners

Some natural compounds may help regulate hematocrit and improve blood flow:
- Grapefruit & Naringin – May reduce hematocrit in some individuals.
- Curcumin (Turmeric) – Has mild blood-thinning properties.
- Fish oil & Omega-3s – Supports cardiovascular health and helps maintain proper blood viscosity.
6. Optimize Sleep And Oxygen Levels
Conditions such as sleep apnea can exacerbate hematocrit increases by reducing oxygen levels, triggering the body to produce more RBCs.
- If experiencing snoring, daytime fatigue, or poor sleep, consider a sleep apnea evaluation.
- Proper CPAP use or lifestyle adjustments (weight loss, sleeping position changes) can lower hematocrit in affected individuals.
When Is Blood Donation Actually Necessary?
While avoiding unnecessary blood donation is ideal, there are cases where it may be required:
- If hematocrit exceeds 57% and symptoms such as dizziness, shortness of breath, or high blood pressure occur.
- If blood viscosity markers indicate a potential clotting risk (e.g., elevated platelets, fibrinogen, or CRP).
- If all other strategies fail to control hematocrit levels safely.
Final Takeaways
- Blood donation should not be the first solution for high hematocrit.
- Increasing injection frequency and staying hydrated are two of the most effective ways to manage hematocrit naturally.
- Dietary adjustments and light cardio can further help stabilize hematocrit levels.
- Sleep apnea and oxygen levels should be considered if hematocrit remains elevated despite other interventions.
- Blood donation is only necessary in extreme cases where symptoms and additional blood markers indicate potential risk.
By implementing these strategies, TRT users can manage hematocrit effectively without the downsides of frequent blood donation. In the next chapter, we’ll discuss blood donation in more detail and when it is actually needed.
Chapter 7: Blood Donation – When It’s Necessary and When It’s Not
Blood donation is often presented as the go-to solution for high hematocrit on TRT, but is it always necessary? Many TRT users are told to donate blood as soon as their hematocrit exceeds 52-54%, yet this recommendation is often outdated and unnecessary. In this chapter, we will explore when blood donation is truly needed, when it should be avoided, and how to determine if it’s the right step for you.
Does Blood Donation Actually Help?
Blood donation can temporarily lower hematocrit, but it is not a permanent solution. Many TRT users find that their hematocrit rebounds within weeks, leading to a cycle of frequent donations without addressing the root cause.
Situations Where Blood Donation Can Be Beneficial:
- Hematocrit above 57% with symptoms – If dizziness, headaches, high blood pressure, or shortness of breath occur.
- Blood viscosity markers indicate risk – Elevated platelets, fibrinogen, or CRP alongside high hematocrit.
- Doctor’s recommendation based on full bloodwork assessment – A qualified TRT-literate doctor should assess all factors, not just hematocrit.
Situations Where Blood Donation May NOT Be Necessary:
- No symptoms despite hematocrit over 54% – High hematocrit alone is not dangerous unless other risk factors are present.
- Stable platelet count and normal blood viscosity markers – If clotting factors are normal, blood thickness is not automatically a concern.
- Frequent blood donation causing iron depletion – Low ferritin levels can lead to chronic fatigue and poor oxygen transport.
How To Donate Blood Correctly (If Needed)
If you and your doctor determine that blood donation is necessary, follow these best practices:
- Opt for whole blood donation – Plasma donation does not effectively reduce hematocrit.
- Space out donations properly – Donating every 8-12 weeks prevents excessive iron loss.
- Monitor ferritin and iron levels – Avoid depleting these critical nutrients.
- Stay hydrated before and after donation – Ensures proper recovery and prevents dizziness.
The Risk of Over-Donating
Excessive blood donation can lead to:
- Iron deficiency and low ferritin levels – Causing fatigue, weakness, and reduced exercise performance.
- Reduced oxygen transport – Lower iron means less hemoglobin production, leading to potential anemia.
- Unnecessary disruption of TRT balance – Frequent donations may cause hormonal fluctuations due to shifts in red blood cell production.
Alternatives to Blood Donation
For those who do not need to donate blood but still want to manage hematocrit, consider:
- Increasing injection frequency to avoid peaks that stimulate excessive erythropoiesis.
- Improving hydration to ensure blood viscosity remains balanced.
- Incorporating light cardio to enhance blood flow and plasma volume.
- Monitoring platelet count and inflammation markers before assuming hematocrit alone is an issue.
Final Takeaways
- Blood donation is not a one-size-fits-all solution for high hematocrit on TRT.
- Hematocrit above 54% does not automatically mean you need to donate blood.
- Assessing symptoms, platelet count, and blood viscosity markers is crucial before deciding.
- Frequent donation can cause iron depletion and long-term health issues.
- Alternative strategies exist to manage hematocrit without unnecessary blood loss.
Understanding when blood donation is necessary—and when it isn’t—ensures TRT users take the right steps for their health without falling into the trap of excessive and unneeded interventions. In the next chapter, we’ll discuss how to find a doctor who understands TRT and hematocrit management properly.
Chapter 8: Finding a Doctor Who Understands Hematocrit and TRT

Not all doctors understand how to properly manage hematocrit on TRT. Many rely on outdated guidelines, overreact to lab numbers, or lack the experience to differentiate between TRT-induced erythrocytosis and true polycythemia. Finding the right doctor is essential for ensuring your TRT protocol is optimized without unnecessary interventions.
Why Many Doctors Misinterpret Hematocrit on TRT
The primary issue with medical management of hematocrit on TRT is that many doctors apply general population guidelines instead of understanding the specific effects of testosterone on red blood cell production. Common mistakes include:
- Assuming hematocrit over 52-54% is always dangerous – Failing to account for symptoms and other blood markers.
- Treating TRT-induced erythrocytosis like polycythemia vera – These are not the same condition, yet many doctors conflate the two.
- Forcing unnecessary blood donations – Overprescribing phlebotomy leads to iron depletion and other issues.
- Ignoring alternative strategies – Some doctors overlook hydration, injection frequency adjustments, and other ways to manage hematocrit.
How to Identify a TRT-Literate Doctor
Finding a doctor who understands TRT and hematocrit requires looking for key indicators that they are well-versed in hormone optimization. Here’s what to consider:
1. They Treat Symptoms, Not Just Numbers
A good TRT doctor does not panic over a single hematocrit reading. Instead, they:
- Assess hematocrit in context (platelet count, blood viscosity, symptoms, etc.).
- Understand that TRT-induced hematocrit increases are normal and not automatically dangerous.
- Avoid knee-jerk reactions like stopping TRT or forcing blood donation.
2. They Understand Alternative Hematocrit Management Strategies
Instead of immediately suggesting blood donation, a TRT-literate doctor will explore:
- Increasing injection frequency to smooth out peaks.
- Monitoring hydration to ensure hematocrit isn’t falsely elevated.
- Checking platelet count and clotting factors before assuming hematocrit alone is a risk.
- Evaluating sleep apnea if hematocrit remains elevated despite adjustments.
3. They Are Open to Discussing Studies and Evidence-Based TRT Protocols
A knowledgeable doctor should be able to reference:
- Studies showing that hematocrit levels up to 54-57% are not inherently dangerous.
- The difference between polycythemia vera and TRT-induced erythrocytosis.
- Alternative options to manage hematocrit without unnecessary interventions.
4. They Do Not Have an Anti-TRT Bias
Some doctors still believe outdated myths about TRT, assuming it is inherently risky. A good TRT provider:
- Recognizes the legitimate benefits of TRT for men with low testosterone.
- Does not have an arbitrary policy of stopping TRT due to a hematocrit number.
- Works with the patient to optimize treatment rather than making uninformed decisions.
Where to Find a Knowledgeable TRT Doctor
If your current doctor does not understand TRT and hematocrit management, consider seeking out specialists in hormone therapy. Options include:
- Hormone Replacement Therapy (HRT) Clinics – Many private clinics specialize in TRT and understand hematocrit management better than general practitioners.
- Online TRT Telemedicine Services – Some reputable providers offer consultations with TRT-literate doctors remotely.
- Patient Forums and TRT Communities – Many experienced TRT users share their doctor recommendations in online groups.
- Functional Medicine Doctors and Endocrinologists – Some endocrinologists and functional medicine practitioners take a more modern approach to TRT.
What to Do if Your Doctor Refuses to Work with You
If your doctor is unwilling to properly manage your TRT, you may need to:
- Educate them – Provide studies and research explaining TRT-induced erythrocytosis.
- Get a second opinion – Another doctor may be more open to reviewing your case.
- Find a new provider – If your doctor refuses to work with you despite clear evidence, seeking a new doctor is often the best choice.
Final Takeaways
- Many doctors misunderstand hematocrit on TRT, leading to unnecessary interventions.
- A knowledgeable TRT doctor treats symptoms, not just numbers.
- Alternative hematocrit management strategies should be considered before recommending blood donation.
- Finding a TRT-literate doctor ensures your treatment is optimized safely and effectively.
Working with the right doctor makes all the difference in managing hematocrit on TRT correctly. In the next chapter, we will cover frequently asked questions related to hematocrit and TRT to clarify common concerns.
Chapter 9: Frequently Asked Questions (FAQ)
When it comes to hematocrit and TRT, misinformation and confusion are common. Many TRT users worry about their hematocrit levels based on outdated or incorrect medical advice. This chapter addresses the most frequently asked questions to provide clarity and practical solutions.
1. At What Level Should I Actually Be Worried About Hematocrit?
Hematocrit alone is not always a cause for concern. While many doctors panic at levels above 52-54%, expert opinions suggest that levels up to 54-57% are often well-tolerated without symptoms. Risk assessment should always include platelet count, blood viscosity, and symptoms, rather than relying on a single number.
2. Will My Hematocrit Go Down If I Stop TRT?
Yes, stopping TRT will eventually lower hematocrit, but this is not a practical solution unless there are serious health concerns. The key is to optimize TRT protocol (e.g., increasing injection frequency, improving hydration) rather than discontinuing treatment unnecessarily.
3. What’s the Fastest Way to Lower Hematocrit Without Donating Blood?
If you want to manage hematocrit without donating blood, consider:
- Increasing injection frequency to avoid large testosterone peaks.
- Staying hydrated to prevent artificially high readings.
- Incorporating light cardio to maintain proper blood flow.
- Reducing excess iron intake from diet and supplements.
- Checking for sleep apnea, which can contribute to elevated hematocrit.
4. Do I Need to Donate Blood Every Time My Hematocrit Is High?
No. Blood donation should not be a routine solution unless hematocrit levels exceed 57% with symptoms or blood viscosity markers indicate increased clotting risk. Unnecessary donations can cause iron depletion, fatigue, and long-term health issues.
5. Does Testosterone Cypionate Increase Hematocrit More Than Other Esters?
All testosterone esters can increase hematocrit, but injection frequency plays a bigger role than ester type. Longer injection intervals (e.g., weekly or biweekly) lead to larger peaks and troughs, which can drive hematocrit higher. Switching to more frequent injections (e.g., daily or every other day) can help stabilize levels.
6. Will Taking Aspirin Help Manage Hematocrit?
Aspirin does not lower hematocrit, but it may help with blood viscosity by reducing platelet aggregation. However, it should not be relied upon as a primary solution, especially without medical supervision.
7. Is There a Connection Between High Hematocrit and Estrogen Levels?
Estrogen plays a role in red blood cell regulation, but it does not directly cause hematocrit increases. Managing estrogen levels properly may contribute to better overall blood health, but lowering estrogen too much can have negative cardiovascular effects.
8. Should I Worry About Blood Clot Risks on TRT?
A high hematocrit alone does not automatically increase clotting risk. Platelet function, fibrinogen levels, and overall blood viscosity are more important factors. Many individuals live at high altitudes with hematocrit levels above 55% without increased clotting risk.
Final Takeaways
- Hematocrit above 54% is not necessarily dangerous—context matters.
- Stopping TRT is not necessary to manage hematocrit levels.
- Blood donation is only needed in extreme cases, not as a routine fix.
- Adjusting TRT protocol, hydration, and lifestyle factors can help regulate hematocrit naturally.
- Clotting risk is not solely determined by hematocrit—other blood markers must be evaluated.
By understanding these FAQs, TRT users can make informed decisions about their hematocrit levels without falling victim to common misconceptions. In the next chapter, we’ll summarize the key takeaways from this guide and how to apply them effectively to your TRT protocol.
Chapter 10: Conclusion – Understanding Hematocrit in the Big Picture
Hematocrit is often misunderstood in the TRT community, with many individuals and even medical professionals overreacting to laboratory numbers without considering the full context. Throughout this guide, we have clarified the misconceptions, provided evidence-based recommendations, and explored the best strategies for managing hematocrit effectively on TRT.
Key Takeaways
1. Elevated Hematocrit on TRT Is Normal
Testosterone naturally stimulates red blood cell production, leading to a higher hematocrit. This does not mean that TRT users are at immediate risk of clotting or cardiovascular issues. The key is understanding the difference between TRT-induced erythrocytosis and true polycythemia vera.
2. Numbers Alone Don’t Define Risk
Hematocrit levels must be evaluated in context with other markers:
- Platelet count – High platelets increase clotting risk far more than hematocrit alone.
- Blood viscosity markers – Fibrinogen, ESR, and CRP help determine actual blood thickness.
- Oxygen saturation – Individuals at high altitudes naturally have hematocrit levels above 55% without negative effects.
3. When to Be Concerned
Hematocrit itself is not dangerous unless accompanied by symptoms like:
- Persistent high blood pressure
- Frequent headaches or dizziness
- Shortness of breath or vision changes
A hematocrit level between 54-57% is not automatically dangerous, but levels exceeding 57% with symptoms require further evaluation.
4. How to Manage Hematocrit Effectively
Instead of defaulting to blood donation, consider these strategies:
- Increase injection frequency – Smaller, more frequent doses help minimize peaks that drive erythropoiesis.
- Optimize hydration – Proper fluid intake prevents falsely elevated hematocrit readings.
- Incorporate light cardio – Regular exercise improves circulation and blood flow.
- Monitor iron levels – Avoid unnecessary blood donation, which can deplete ferritin and cause fatigue.
- Assess for sleep apnea – Low oxygen levels from sleep apnea can trigger excessive RBC production.
5. Work with the Right Doctor
Not all doctors understand TRT-induced hematocrit changes. A knowledgeable physician will:
- Assess symptoms instead of overreacting to a lab number.
- Consider all blood markers before recommending interventions.
- Use evidence-based strategies instead of outdated fear-driven approaches.
Final Thoughts
TRT users should be empowered with knowledge instead of driven by fear. High hematocrit is a natural physiological response to testosterone, and when managed properly, it is rarely a cause for concern. The key is understanding when action is necessary and when it is not.
By applying the insights from this guide, you can take control of your TRT journey with confidence, ensuring optimal health and well-being without unnecessary interventions.